Organ-on-a-Chip Mimics Human Gut Action
In partnership with the University of Luxembourg, scientists at the University of Arizona College of Medicine – Phoenix have developed a new instrument for studying a biological model of the human gastrointestinal tract that mimics the actual conditions and processes that occur within the intestine.
The research, published earlier this month in Nature Communications, will allow scientists to see how cells from individuals respond to certain drugs, allowing them to formulate personalized drug therapies. With the organ-on-a-chip technology, researchers can analyze the complex interactions between human cells and the microbial ecosystems of the gut, predicting their effects on health or disease onset, and study the action of probiotics, nutritional compounds or drugs.

HuMiX allows researchers to determine interactions with several drugs at a time and could replace the animal model, Zenhausern said. “The mice model is not a good representation of the complex human gut biology,” he said. The combination of functional plastic microfluidic devices and nanofabricated membranes will also provide a modular technology platform for further sensing and assembling different types of biological components, such as immune or neuronal cells into various tissues or organs, he said.
"The UA team is designing biological systems for studying the impact of the gut-brain axis, which may be involved in cognition, but also in Alzheimer’s or Parkinson’s diseases,” Zenhausern said.
The Center for Applied NanoBioscience and Medicine’s staff of a dozen scientists finds applications and creates devices for a new generation of biological tools and sensors based on nano- and microscale technologies.
With the HuMiX model, Paul Wilmes, PhD, senior author of the research and principal investigator at the Luxembourg Center, said scientists can actually look at responses of human cells in relation to specific microbiome compositions. “It’s a model that is much more relevant from a human disease and health perspective,” he said.
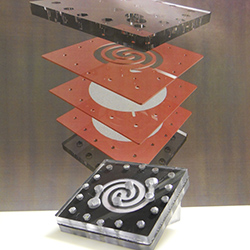
The core of the technology is a spiral-shaped nanofabricated chamber that has a thin, permeable polymer membrane separating bacteria and nutrients from human gastrointestinal cells, while still allowing communication between the layers.
The practical implications allow scientists to look at how different diets, along with different microbiome compositions, might affect human cell physiology.
“We can put in (to the model) cells from individuals and see how those cells respond to certain drugs and start really understanding how we might formulate drug therapies in a very personalized way,” Wilmes said.
Zenhausern said the development of tools for better characterizing the functional role of the human microbiome in human health has the potential to aid in the discovery of new treatments for obesity, inflammatory bowel disease, diabetes, cancer and neurodegenerative diseases. The technology also could be a valuable tool for better understanding the role of microbials in the physical performance and cognitive function of soldiers in war, athletes or other professionals under high-stress activities.
For their tests confirming the validity of HuMiX experiments, researchers used pure cultures of various bacterial strains. They then studied how the gene activity and metabolism of intestinal epithelial cells changed, depending on the bacterial strain. A comparison of data from HuMiX with other research groups who obtained their data from humans or animals showed strong agreement, meaning HuMiX delivered an accurate portrayal of the cellular and molecular processes taking place in the human gut.
Media Contact:
Marian Frank
Phone: 602-827-2022
About the College
Founded in 2007, the University of Arizona College of Medicine – Phoenix inspires and trains exemplary physicians, scientists and leaders to optimize health and health care in Arizona and beyond. By cultivating collaborative research locally and globally, the college accelerates discovery in a number of critical areas — including cancer, stroke, traumatic brain injury and cardiovascular disease. Championed as a student-centric campus, the college has graduated more than 900 physicians, all of whom received exceptional training from nine clinical partners and more than 2,700 diverse faculty members. As the anchor to the Phoenix Bioscience Core, which is projected to have an economic impact of $3.1 billion by 2025, the college prides itself on engaging with the community, fostering education, inclusion, access and advocacy.


