
Cervical Cancer May Be Driven by Imbalance in Vaginal Bacteria, UA Research Finds

Virtually all cervical cancers are caused by HPV, or human papillomavirus, dubbed the “common cold” of sexually transmitted infections because nearly every sexually active person catches it. Fortunately, the immune system vanquishes the majority of HPV infections, with only a small percentage progressing to precancer and, ultimately, cancer. But why do some people clear the infection while others are unable to fight it?
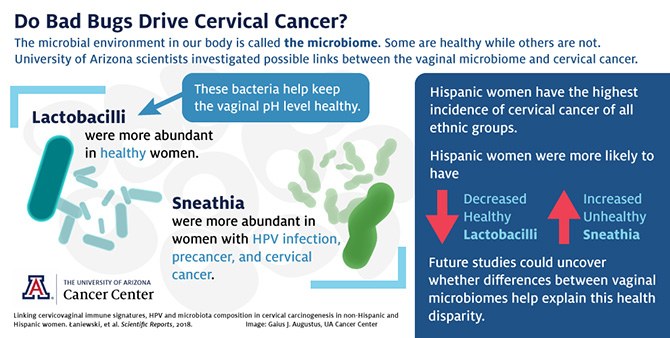
Her team found that women without cervical abnormalities are hosts to different communities of vaginal bacteria than women with cervical cancer and precancer, a discrepancy that reveals a direct relationship between “good” bacteria and cervical health, and “bad” bacteria and increased cancer risk. The results were published online May 15 in the open-access Nature publication Scientific Reports.
The microbiome is the community of microbes that take up residence in the body. Some species of bacteria — such as lactobacilli, which are related to but distinct from the probiotics found in yogurt — have been found to promote a healthy vaginal environment. For example, previous research revealed women with Lactobacillus gasseri-dominant vaginal microbiomes are more likely to clear HPV infections. Good bacteria also can hold territory to keep bad bacteria from moving in. Sometimes, however, they lose this turf war.
“In cancer and precancer patients, lactobacilli — good bacteria — are replaced by a mixture of bad bacteria,” said Dr. Herbst-Kralovetz. In the study, as Lactobacillus populations dwindled, cervical abnormalities became more severe. On the other hand, bad bacteria, called Sneathia, were linked to HPV infection, precancer and cervical cancer.
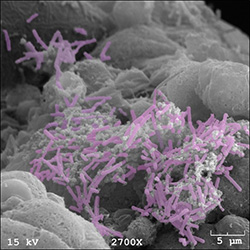
Sneathia are rod-shaped bacteria that can grow into fibrous chains. They have been associated with other gynecological conditions, including bacterial vaginosis, miscarriage, preterm labor, HPV infection and cervical precancer. Dr. Herbst-Kralovetz’s study is the first to find that a substantial Sneathia population is associated with all stages of the HPV-to-cancer continuum, from initial HPV infection to precancer to invasive cervical cancer.
What’s unknown is whether Sneathia species actively promote HPV infection or cancer formation, or if they’re just along for the ride. The current study offers only a snapshot of women at one point in time. To establish a cause-and-effect relationship, future studies must follow women over time.
“There’s really not a lot in the literature about how Sneathia functions in the reproductive tract,” said Dr. Herbst-Kralovetz. “How Sneathia may be impacting the hallmarks of cancer is an active area of investigation in our lab.”
The bacteria that make up the vaginal microbiome are inextricably linked to the acidity of the vaginal environment. A vagina with a pH of 4.5 or below defends against harmful bacteria that are unable to survive in such an acidic environment. When pH is elevated, harmful bacteria gain the opportunity to move in, disrupting the vaginal ecosystem.
“High pH is a great reflection of the vaginal microbiome composition,” said Dr. Herbst-Kralovetz. “Lactobacilli produce lactic acid that directly lowers the pH. If you have high levels of lactobacilli, you’re going to have a lower vaginal pH, and that’s associated with health.”
Dr. Herbst-Kralovetz’s team found that, as the vaginal environment loses acidity, cervical abnormalities become more severe. The team is the first to show a relationship between elevated pH and advanced cervical abnormalities.
Roughly half of the patients studied were Hispanic, while the other half were of non-Hispanic origin. Hispanic women have the highest incidence of cervical cancer of all racial and ethnic groups, according to the National Cancer Institute. Studies assessing factors such as race and ethnicity in cancer risk are important for understanding why some populations are disproportionately affected by cancer.
“I wanted to truly reflect the Arizona population in our study,” said Dr. Herbst-Kralovetz. “Latinas are at a higher risk of cervical cancer. A long-term goal of mine is to help address that health disparity.”
The team found that Hispanic women were more likely to have decreased Lactobacillus populations and increased Sneathia populations. Perhaps differences in the vaginal microbiome is one factor behind Hispanic women’s increased risk for cervical cancer.
“One of our duties at the UA Cancer Center is to improve the health of Arizonans,” said William Cance, MD, deputy director of the UA Cancer Center at Dignity Health St. Joseph’s Hospital and Medical Center. Referring to the UA’s recent designation as a Hispanic Serving Institution by the U.S. Department of Education, Dr. Cance added, “Studies such as those being led by Dr. Herbst-Kralovetz show our commitment to supporting not just the education of Hispanics in Arizona, but also their health.”
“This was a highly collaborative group, performing a multi-site study here in the Phoenix area,” concluded Dr. Herbst-Kralovetz. “This work serves as the foundation for a lot of other studies. It creates many hypotheses and future directions for us in the lab, and also allows us to address some of these health disparities here in Arizona.”
Article By: Anna C. Christensen, UA Cancer Center
This study was supported by the Flinn Foundation Grant No. 1917 and partially by the National Institutes of Health NIAID Grant 1R15AI113457-01A1 and the National Institutes of Health NCI Grant P30 CA023074. The study was conducted at the UA Cancer Center at Dignity Health St. Joseph’s Medical Center and Maricopa Integrated Health Systems.
About the College
Founded in 2007, the University of Arizona College of Medicine – Phoenix inspires and trains exemplary physicians, scientists and leaders to advance its core missions in education, research, clinical care and service to communities across Arizona. The college’s strength lies in our collaborations and partnerships with clinical affiliates, community organizations and industry sponsors. With our primary affiliate, Banner Health, we are recognized as the premier academic medical center in Phoenix. As an anchor institution of the Phoenix Bioscience Core, the college is home to signature research programs in neurosciences, cardiopulmonary diseases, immunology, informatics and metabolism. These focus areas uniquely position us to drive biomedical research and bolster economic development in the region.
As an urban institution with strong roots in rural and tribal health, the college has graduated more than 1,000 physicians and matriculates 130 students each year. Greater than 60% of matriculating students are from Arizona and many continue training at our GME sponsored residency programs, ultimately pursuing local academic and community-based opportunities. While our traditional four-year program continues to thrive, we will launch our recently approved accelerated three-year medical student curriculum with exclusive focus on primary care. This program is designed to further enhance workforce retention needs across Arizona.
The college has embarked on our strategic plan for 2025 to 2030. Learn more.