
Traumatic Brain Injury Survival Doubled by Pre-Hospital Treatment

The implementation of a massive, statewide public health initiative led by University of Arizona researchers and involving 21,000 pre-hospital care patients has doubled the survival rate of severe traumatic brain injury victims and tripled the survival rate among those who were intubated.
The Excellence in Pre-hospital Injury Care Project, or EPIC, is the first major pre-hospital interventional project to evaluate the impact of national pre-hospital traumatic brain injury, or TBI, treatment guidelines, which were developed after years of research but contradicted decades of anecdotal protocol.
"Science has finally caught up. We’re finding the right benchmarks to go after," said Sean Culliney, an EMS training coordinator at the Northwest Fire District in Tucson. "In my 20 years, what I’ve learned has been turned on its head."
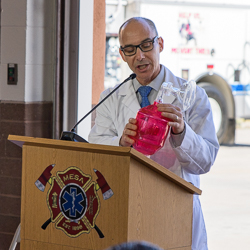
"A TBI initiative of this scale has never been attempted by pre-hospital providers," said Ben Bobrow, MD, distinguished professor of Emergency Medicine at the UA and a co-author on the study, which was published May 8 in JAMA Surgery: The Journal of the American Medical Association.
UA researchers spearheaded the EPIC initiative in partnership with the Arizona Department of Health Services and more than 130 fire departments and pre-hospital emergency medical service, or EMS, agencies across the state. The project was funded by a $3.6 million grant from the National Institute of Neurological Disorders and Stroke, or NINDS, part of the National Institutes of Health.
More than 11,000 Arizona paramedics and emergency medical technicians, or EMTs, have been trained in the new treatment protocol since 2012.
"Partnerships like this one are such an important way for the UA to serve Arizona and advance medicine worldwide," said UA President Robert C. Robbins. "Fifteen years ago, the University of Arizona was instrumental in the push to implement compression-only CPR, which has been revolutionary for emergency medicine. I am so proud to see the UA's excellence in innovation and tradition of improving upon accepted practices continues with Dr. Spaite and his team. This TBI initiative could save countless lives, and I am thrilled by what this will allow our first responders to do for their patients."
"Arizona is once again leading the nation in managing groundbreaking medical research that will improve how emergency responders treat people with traumatic brain injuries," said Arizona Gov. Doug Ducey. "Thanks to the work of the University of Arizona, the Arizona Department of Health Services and our state's entire EMS system, we have made a huge step forward in protecting the lives of people in Arizona and the entire nation."
The 'Three H-Bombs'
Through EPIC, first responders are taught to treat and prevent the "Three H-bombs:" hyperventilation, hypoxia and hypotension.
Prior to the implementation of EPIC, first responders were taught to hyperventilate people with a TBI. Using an air bag with an opening placed over the mouth or directly into the windpipe, medics would squeeze air into the lungs quickly and deeply. Doing so reduces potentially deadly pressure in the brain, which was thought to be helpful. However, recent research has shown that while hyperventilation lowers intracranial pressure, it also deprives the brain of blood and oxygen.
After four minutes of low flow, neurons start to die.
Research shows first responders naturally tend to breathe patients far too many times a minute, leading to hyperventilation, according to Culliney. As a result, agencies now use breathing bags with a light that flashes at the proper rate, serving as a visual cue.
"What EPIC found was that the pre-hospital care is powerfully synergistic with critical care and surgical care in the hospital," Spaite said. "If we deliver a person whose brain is going to die, it doesn’t matter how good the trauma team is, we will never get those neurons back."
EMTs can prevent the second "H-Bomb" — hypotension, or low blood pressure — by quickly administering intravenous fluids to TBI patients.
The last "H-Bomb" is hypoxia, which deprives the brain of oxygen and kills neurons. To combat hypoxia, first responders are taught to place high-flow oxygen on patients as soon as possible.
"This demonstrates the significance of conducting studies in real-world settings and brings a strong evidence base to the guidelines," said Patrick Bellgowan, program director at NINDS. "It suggests we can systematically increase the chances of saving lives of thousands of people who suffer severe traumatic brain injuries."

This work was supported by the NINDS (NS071049).
Researcher Contact:
Dan Spaite
UA Department of Emergency Medicine
520-626-2156
Media Contact:
Mikayla Mace
University Communications
520-621-1878
About the College
Founded in 2007, the University of Arizona College of Medicine – Phoenix inspires and trains exemplary physicians, scientists and leaders to advance its core missions in education, research, clinical care and service to communities across Arizona. The college’s strength lies in our collaborations and partnerships with clinical affiliates, community organizations and industry sponsors. With our primary affiliate, Banner Health, we are recognized as the premier academic medical center in Phoenix. As an anchor institution of the Phoenix Bioscience Core, the college is home to signature research programs in neurosciences, cardiopulmonary diseases, immunology, informatics and metabolism. These focus areas uniquely position us to drive biomedical research and bolster economic development in the region.
As an urban institution with strong roots in rural and tribal health, the college has graduated more than 1,000 physicians and matriculates 130 students each year. Greater than 60% of matriculating students are from Arizona and many continue training at our GME sponsored residency programs, ultimately pursuing local academic and community-based opportunities. While our traditional four-year program continues to thrive, we will launch our recently approved accelerated three-year medical student curriculum with exclusive focus on primary care. This program is designed to further enhance workforce retention needs across Arizona.
The college has embarked on our strategic plan for 2025 to 2030. Learn more.