New Study to Explore Link Between Hypertension Treatment and Development of Heart Failure
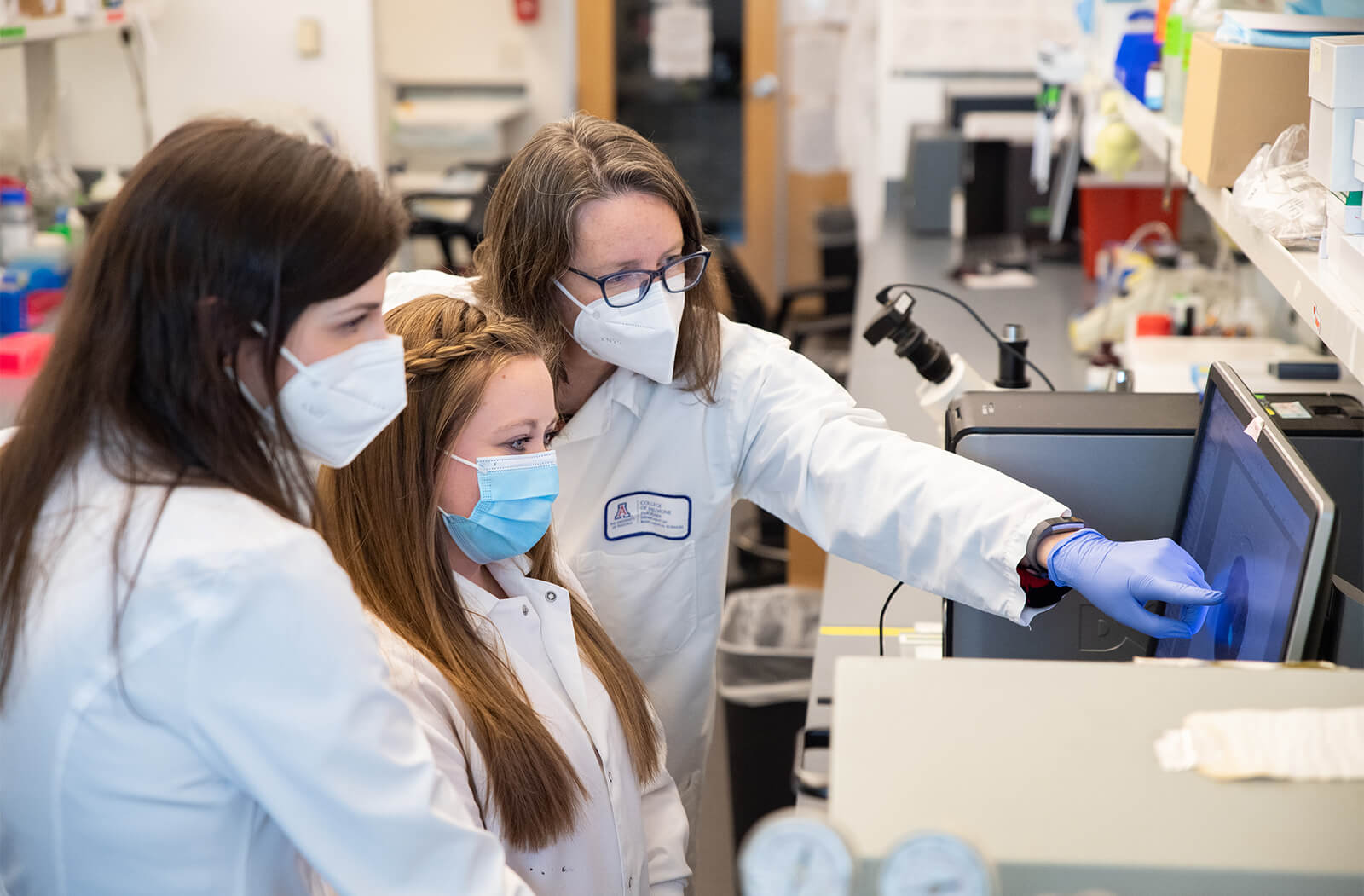
Researchers at the University of Arizona College of Medicine – Phoenix have received a grant to study how medications used to treat hypertension may provide insight into novel treatments to produce long-lasting protection against heart disease.
Taben Hale, PhD, is the director of the Hale Laboratory at the U of A College of Medicine – Phoenix. She will lead the study, “Targeting Resident Cardiac Fibroblast Subpopulations for Protection Against Fibrosis,” with R01 grant funding from the National Institutes of Health (NIH).
Hypertension, also known as high blood pressure, is a major risk factor for development of heart failure. Hypertension stimulates activation of cardiac fibroblasts (CFs) — cells which play a primary role in regulating the production of the extracellular matrix (ECM) — a large network of proteins that helps cells attach to and communicate with each other.
Prolonged activation of CFs due to hypertension stimulates production of growth factors and signaling molecules in these cells, resulting in excessive ECM production. This leads to the development of fibrosis and impairs the heart’s ability to effectively pump blood to the rest of the body.
Potential Long-term Protection Against Fibrosis
Fibrosis is a common end-stage characterization of nearly every type of heart disease. Although there are no approved treatments for cardiac fibrosis, angiotensin-converting enzyme inhibition (ACE inhibitor) medications limit CF activation.

The new study will reveal the mechanisms by which CFs can be shifted to a lower activation state. By limiting CFs’ activation, researchers hope to identify methods to protect against future fibrosis. Researchers seek to determine how changes in the regulation of specific CF genes create a relatively stable phenotype that is less prone to activation.
Researchers hope the new study may contribute to the development of medications that target cardiac fibroblasts to prevent the cardiac remodeling which leads to heart failure.
About the College
Founded in 2007, the University of Arizona College of Medicine – Phoenix inspires and trains exemplary physicians, scientists and leaders to advance its core missions in education, research, clinical care and service to communities across Arizona. The college’s strength lies in our collaborations and partnerships with clinical affiliates, community organizations and industry sponsors. With our primary affiliate, Banner Health, we are recognized as the premier academic medical center in Phoenix. As an anchor institution of the Phoenix Bioscience Core, the college is home to signature research programs in neurosciences, cardiopulmonary diseases, immunology, informatics and metabolism. These focus areas uniquely position us to drive biomedical research and bolster economic development in the region.
As an urban institution with strong roots in rural and tribal health, the college has graduated more than 1,000 physicians and matriculates 130 students each year. Greater than 60% of matriculating students are from Arizona and many continue training at our GME sponsored residency programs, ultimately pursuing local academic and community-based opportunities. While our traditional four-year program continues to thrive, we will launch our recently approved accelerated three-year medical student curriculum with exclusive focus on primary care. This program is designed to further enhance workforce retention needs across Arizona.
The college has embarked on our strategic plan for 2025 to 2030. Learn more.