Pharmacogenomics Symposium Showcased Progress and Potential in the Field
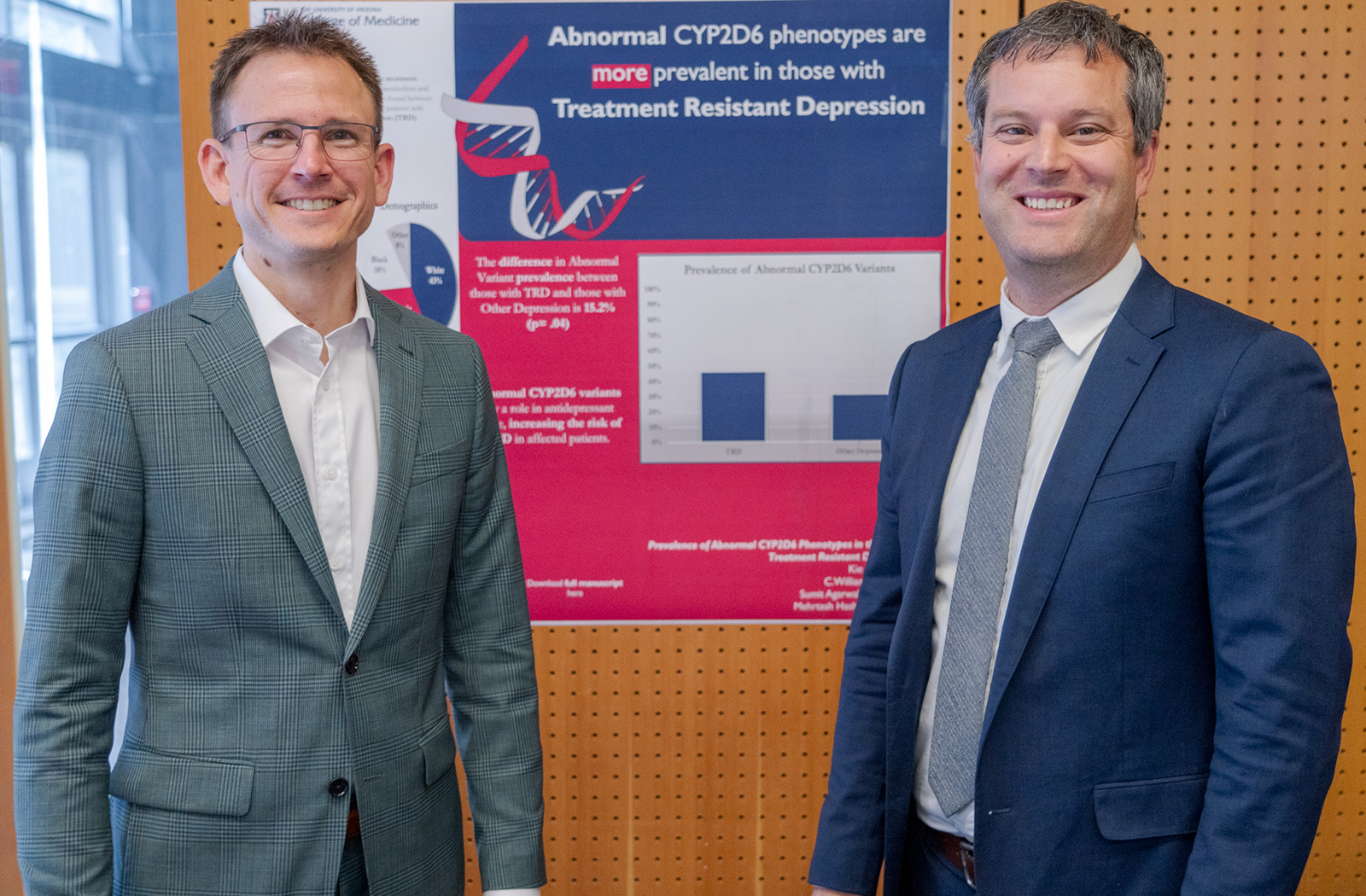
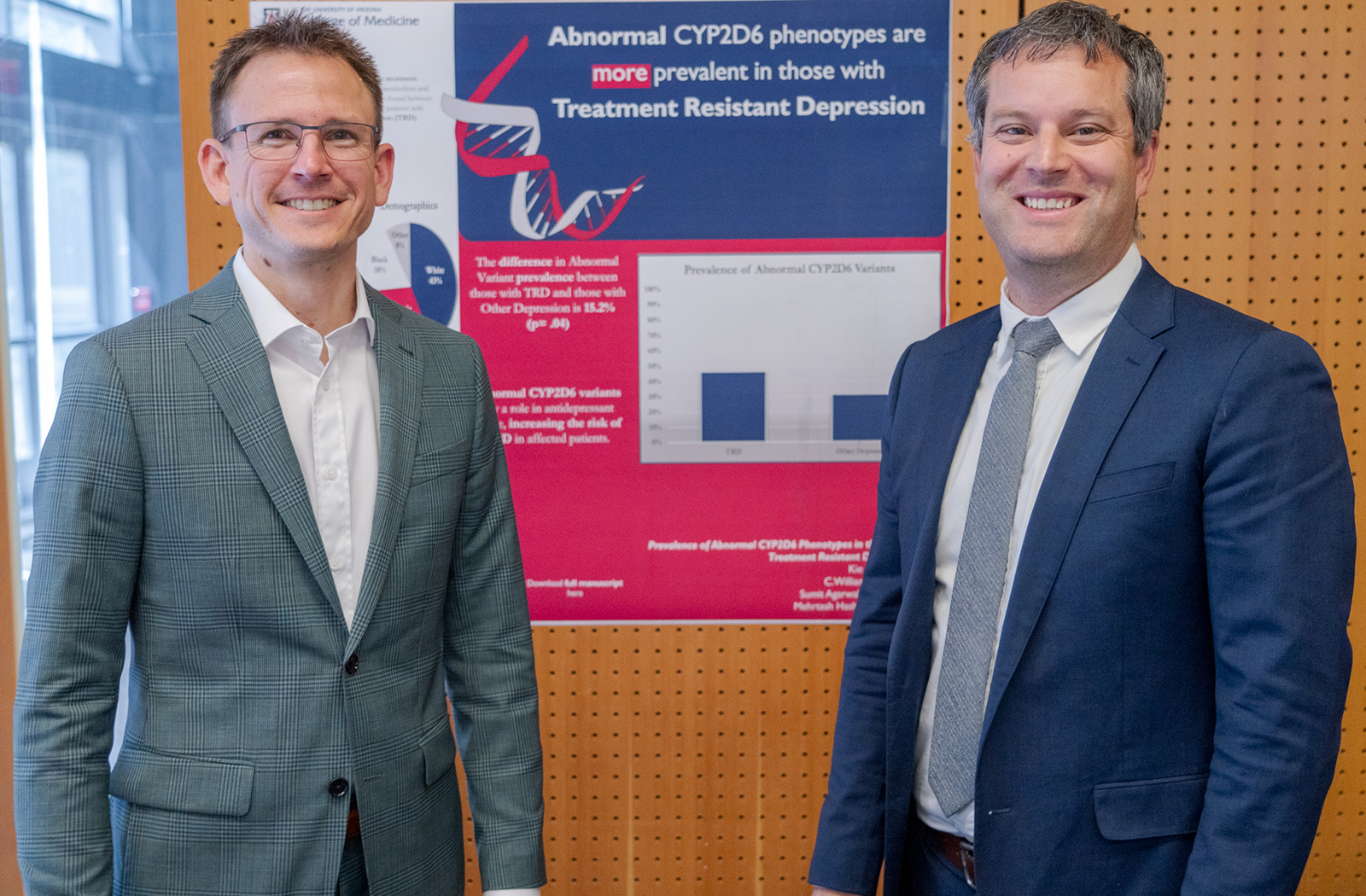
Researchers from across the United States and Canada gathered at the University of Arizona College of Medicine – Phoenix’s campus to discuss recent trends, new therapies and what the future will hold for the field of pharmacogenomics during the annual Precision Medicine and Pharmacogenomics Symposium April 8.
Pharmacogenomics is the study of how genes affect a person’s response to drugs and combines pharmacology and genomics to prescribe effective medications based on a patient’s genetic makeup. Central to the college’s focus on precision medicine, its promise for improved patient outcomes by preventing adverse interactions is why medical students at the college are instructed on the foundational principles of the field.
“One of the key things we have done at the college is implement a precision medicine longitudinal theme with our medical students,” Will Heise, MD, assistant professor at the Division of Clinical Data Analytics and Decision Support at the U of A College of Medicine – Phoenix, said. “Students have been subject to a number of sessions in pharmacogenomics and precision medicine with the goal of providing tools for them to integrate precision medicine into their future practice.”
The symposium is an extension of those efforts; and throughout five oral presentations, members of the audience learned about the latest research on gene-drug interactions. Special topics also included gene-drug interactions in psychiatric conditions, as well as responses in anticoagulant and antiplatelet drugs.

Nita Limdi, PharmD, PhD, MSPH, is a professor of Neurology at the University of Alabama at Birmingham, School of Medicine – Personalized Medicine Institute. Her presentation discussed pharmacogenomics for anticoagulant and antiplatelet response.
Anticoagulants are medicines that help prevent blood clots and are commonly known as blood thinners. People who are at high risk of developing blood clots are prescribed anticoagulants to reduce their chances of developing serious conditions such as stroke, heart attack and pulmonary embolism.
Currently, anticoagulants are the leading cause of medication-related hospitalizations in the United States. Adverse drug reactions are the fourth-leading cause of death, according to the United States Food and Drug Administration.
The aim of Dr. Limdi’s research is to identify common and rare genetic variants on anticoagulation response to examine what other factors affect comorbid conditions and co-medications. These include ancestry, diet, exercise and other medications.
Her team’s goal was to develop and validate polygenic risk scores for 10 diseases across various ancestral groups. The study is almost finished and has recruited 25,000 patients in primary care. Dr. Limdi said that the data collected from patients contains genomics, family history and rich social determinants of health data.
“When reports on genetic testing come in, if the patient has no genetic risk, the providers should still be made aware,” Dr. Limdi said. “If there is a high polygenic risk, providers will call to notify the patient or there is a video visit to explain it.”
Chad Bousman, PhD, works as an associate professor at the University of Calgary’s Department of Medical Genetics in Alberta, Canada. His presentation discussed pharmacogenomics with an emphasis on prescription for psychiatric diseases.

Among the hurdles for conducting pharmacogenomics testing is building provider confidence and determining who should be tested. In regard to working around clinical workflow integration, Dr. Bousman found that there is no correct answer.
“There are so many workflows out there, and I would say that all of them are good for particular settings,” Dr. Bousman said. “The key that I find between a successful workflow and a less successful workflow are the ones that disrupt existing prescribing practice as little as possible.”
The future of pharmacogenomics in psychiatry will continue to grow. According to Dr. Bousman, 64% of the top 25 prescribed psychiatric medications do not have pharmacogenomics guidelines.
“Fluoxetine is the only SSRI that does not have a guideline and is also the first line therapy for depression in adolescents,” Dr. Bousman said. “It’s a huge gap in our ability to implement pharmacogenetic testing in child adolescent psychiatry.”
Vignesh Subbian, PhD, MS, is an associate professor in the University of Arizona Department of Biomedical Engineering and Department of Systems and Industrial Engineering and is a member of the BIO5 Institute.
Dr. Subbian’s presentation focused on past and current work related to patient-centered clinical decision support for pharmacogenomics. He discussed integrating pharmacogenomic testing into electronic health records with clinical decision support and selecting the correct workflow for patients to receive data.
“If you want a holistic pharmacogenomics clinical support, it depends on the knowledge bases,” Dr. Subbian said. “Successful adoption of pharmacogenomics into routine clinical care requires a machine-readable vault of knowledge suitable for use within an electronic health record.”
Tyler Gallo, PharmD, an assistant professor in the Division of Clinical Data Analytics and Decision Support at the college, focused his presentation on the impact and outcomes of pharmacogenomic clinical decision support.

His presentation built upon Dr. Subbian’s talk by providing examples of how clinical decision support is used in the field. Dr. Gallo mentioned that there are two main applications of clinical decision support in pharmacogenomics.
“One is to identify patients who should undergo pharmacogenomic testing, and the other is post-test alerts for when pharmacogenomic testing results in a change or modification of that therapy,” Dr. Gallo said. “Recommendations can change over time, so we need to continually evaluate these things and make sure they’re functioning as intended.”
Dr. Heise’s talk focused on the future of pharmacogenomic clinical decision support and automation.
“We have to consider the opportunity that patients have to be in a place where they can receive precision medicine,” Dr. Heise said. “We recognize we have disparities in delivery of pharmacogenomics, precision medicine and research. Our pharmacogenomic panels are inadequate if we do not address variants in populations.”
Dr. Heise discussed the limitations of AI to provide accurate medical diagnoses and recommended therapeutics. He demonstrated that ChatGPT is useful for background information but not for actual patient care because it lacks updated information and data personalized to the patient.
“What we recognize is that AI, while it can be incredibly helpful and meaningful, is limited, and it will never have human understanding and capacity,” Dr. Heise said. “Many of the strides that have been made in AI are not because we’ve been able to make it more human-like, but rather because we have higher computational power.”
The event was sponsored by the Arizona Biomedical Research Centre and the Flinn Foundation.
About the College
Founded in 2007, the University of Arizona College of Medicine – Phoenix inspires and trains exemplary physicians, scientists and leaders to advance its core missions in education, research, clinical care and service to communities across Arizona. The college’s strength lies in our collaborations and partnerships with clinical affiliates, community organizations and industry sponsors. With our primary affiliate, Banner Health, we are recognized as the premier academic medical center in Phoenix. As an anchor institution of the Phoenix Bioscience Core, the college is home to signature research programs in neurosciences, cardiopulmonary diseases, immunology, informatics and metabolism. These focus areas uniquely position us to drive biomedical research and bolster economic development in the region.
As an urban institution with strong roots in rural and tribal health, the college has graduated more than 1,000 physicians and matriculates 130 students each year. Greater than 60% of matriculating students are from Arizona and many continue training at our GME sponsored residency programs, ultimately pursuing local academic and community-based opportunities. While our traditional four-year program continues to thrive, we will launch our recently approved accelerated three-year medical student curriculum with exclusive focus on primary care. This program is designed to further enhance workforce retention needs across Arizona.
The college has embarked on our strategic plan for 2025 to 2030. Learn more.