Physician Seeks to Improve Training for Brain Death Testing
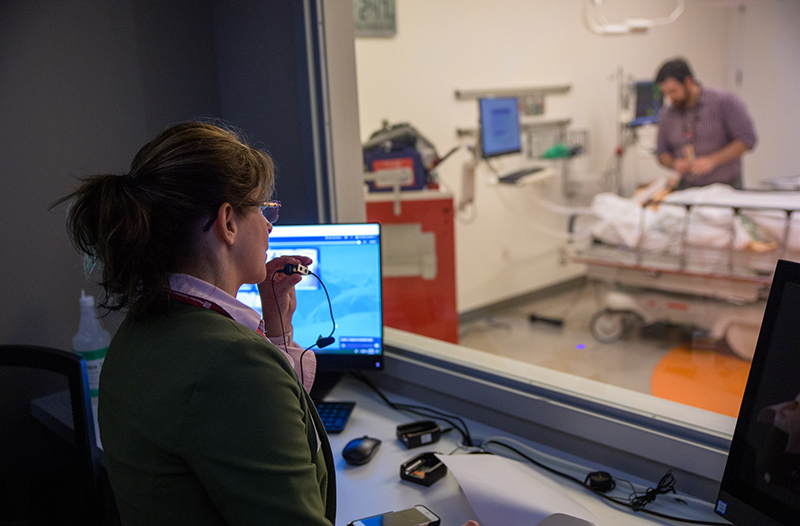
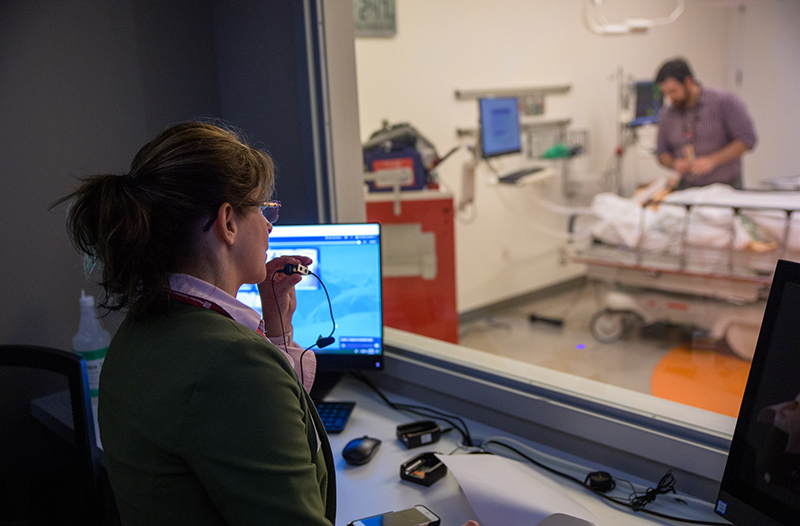
In pediatrics, there is no standard training guideline for doctors to perform brain death exams. Michele Munkwitz, MD, an associate program director of the Critical Care Fellowship at the University of Arizona College of Medicine – Phoenix Division of Pediatric Critical Care at Phoenix Children’s Hospital, is collaborating with the college’s Center for Simulation and Innovation on a three-year study to assess the ability of residents and fellows to improve their skills in performing brain death exams.
As part of the research, the team recently trained about 20 residents and fellows over two days in the simulation center. Sessions included simulation brain death testing as well as training on how to discuss the sensitive topic with a child’s family.
Explain Your Research

Why is This Important?
The brain death exam is used to declare death in patients who have suffered an irreversible loss of entire brain function. Brain death, or death declared with neurologic criteria, is a rare event in pediatrics. There is literature to suggest that Pediatric Critical Care fellows have inconsistent opportunities to perform the exam. It also has been found that the fellows are more comfortable with their skills after they have had six independent opportunities to perform the exam. We hypothesize that, given a consistent opportunity to perform six exams with simulation, trainees will be comfortable with and competent in their exam skills and the ability to communicate with families in this uniquely difficult time.
How Will This Help the Community?
If our hypothesis is true, this study will inform guidelines and standards in brain death examination education. We hope to contribute to increasing trust with families and in the community regarding this diagnosis.
What Has Previous Research Shown?
Previous studies have found increased short-term retention of skills in the exam with a one-time simulation. However, there is no evidence that a one-time simulation increases long-term retention, competence and confidence in skills. This study will evaluate repeated simulations over time and long-term retention and confidence in skills. We base our practice of six simulations on a 2018 study in Pediatric Critical Care Journal that found confidence in exam skills increased after six independent exams.
Why Now?

How Did You Become Interested in this Area of Research?
I have an interest in ethics, as well as medical education. I have been deeply impacted by my own experiences with children who have suffered irreversible loss of their entire brain. It is such a difficult and confusing time for families. It is my hope to improve the process and make the experience better for everyone.
About the College
Founded in 2007, the University of Arizona College of Medicine – Phoenix inspires and trains exemplary physicians, scientists and leaders to advance its core missions in education, research, clinical care and service to communities across Arizona. The college’s strength lies in our collaborations and partnerships with clinical affiliates, community organizations and industry sponsors. With our primary affiliate, Banner Health, we are recognized as the premier academic medical center in Phoenix. As an anchor institution of the Phoenix Bioscience Core, the college is home to signature research programs in neurosciences, cardiopulmonary diseases, immunology, informatics and metabolism. These focus areas uniquely position us to drive biomedical research and bolster economic development in the region.
As an urban institution with strong roots in rural and tribal health, the college has graduated more than 1,000 physicians and matriculates 130 students each year. Greater than 60% of matriculating students are from Arizona and many continue training at our GME sponsored residency programs, ultimately pursuing local academic and community-based opportunities. While our traditional four-year program continues to thrive, we will launch our recently approved accelerated three-year medical student curriculum with exclusive focus on primary care. This program is designed to further enhance workforce retention needs across Arizona.
The college has embarked on our strategic plan for 2025 to 2030. Learn more.