Potential Target to Diagnose, Monitor Cervical Cancer Treatment Aim of U of A Health Sciences Researchers
University of Arizona Health Sciences researchers’ quest to better understand the vaginal microbiome and its role in human papillomavirus (HPV) infection, which may progress into cervical cancer, has revealed potential new targets for early detection and monitoring treatment — proteins known as immune checkpoints.
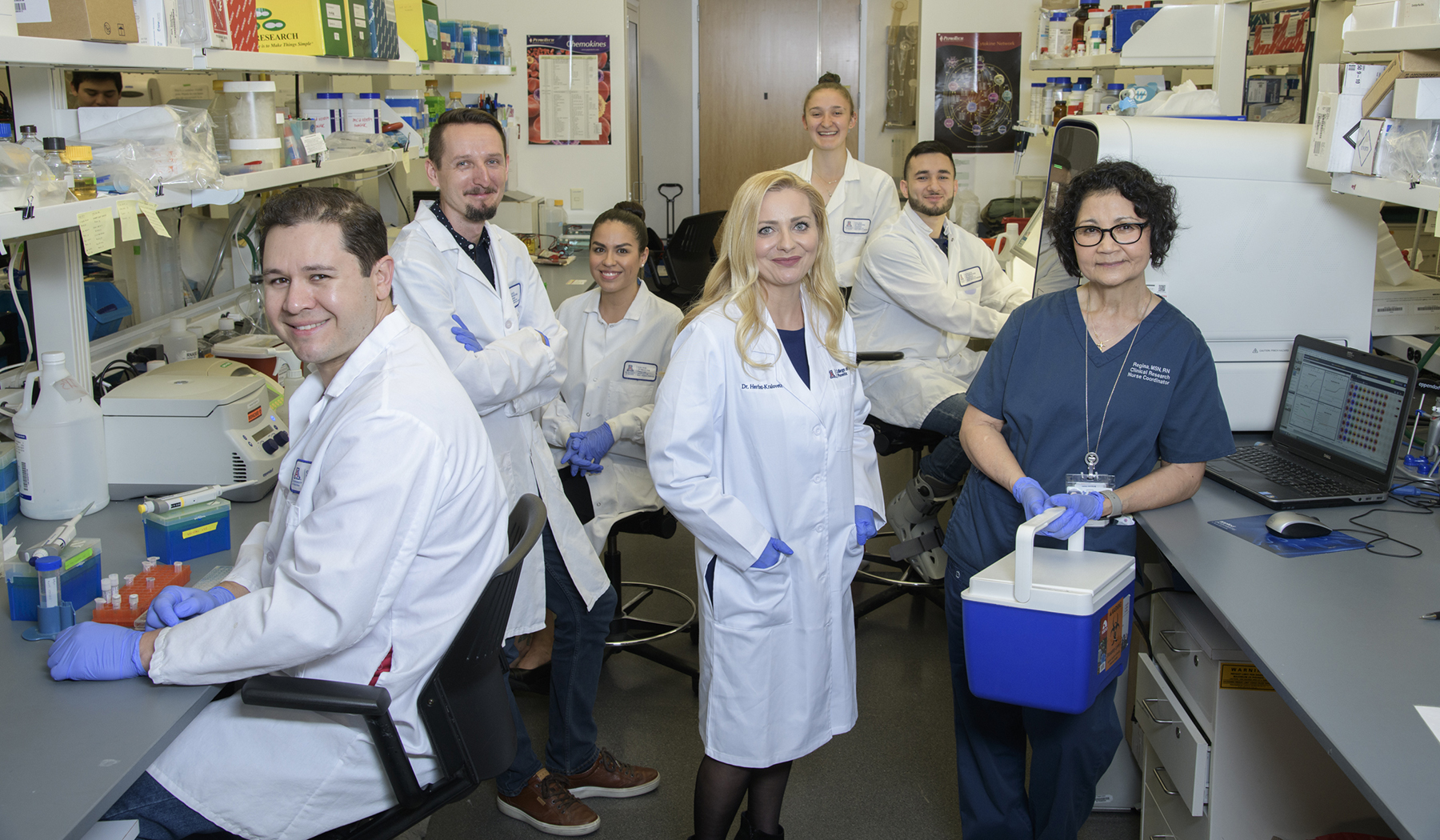
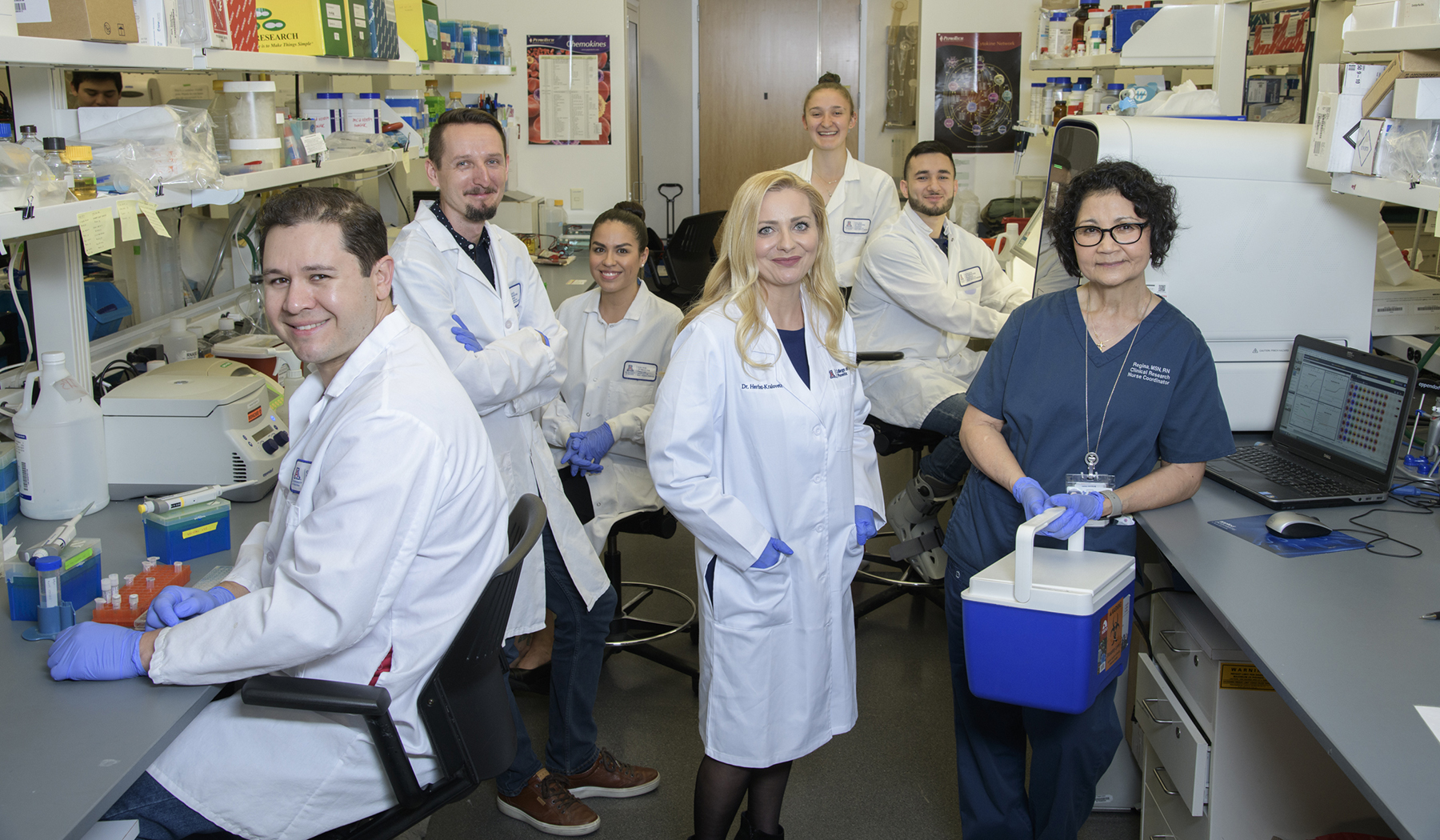
Immune checkpoints regulate a patient’s immune system and can dictate recognition and elimination of cancer cells. Presence and implications of these proteins in the cervicovaginal environment, however, had previously not been studied, said Melissa Herbst-Kralovetz, PhD, associate professor of Basic Medical Sciences and Obstetrics/Gynecology at the U of A College of Medicine – Phoenix , and director of the Women’s Health Research Program, as well as a member of the U of A Cancer Center.

“We know immune checkpoint proteins often are overexpressed in the tumor microenvironment, meaning they are increased, which can promote carcinogenesis (cancer development) by not allowing for an effective anti-tumor response,” Dr. Herbst-Kralovetz said. “So we hypothesized these checkpoints also may be at work in the cervicovaginal microenvironment and may be altered with HPV infection, precancer and cancer.”
In a new study published in August in npj Precision Oncology, a journal of the Nature Publishing Group, and referenced in Nature’s “Behind the Paper” blog, Drs. Herbst-Kralovetz and Laniewski discuss their research in collaboration with colleagues from the U of A Biostatistics Shared Resource, including Denise Roe, DrPH, resource director; Haiyan Cui, PhD , senior research specialist, U of A Cancer Center; and Dana Chase, MD, a clinical collaborator from Arizona Oncology.
Using cervicovaginal lavages (CVLs), a non-invasive method to collect fluid samples from a patient, the researchers were able to measure the immune checkpoint proteins in the cervicovaginal environment. As a result, they discovered these proteins have the potential to predict whether a woman has dysplasia — abnormal cell growth — or cancer.
“We identified immune checkpoints that specifically and sensitively discriminated cancer patients from healthy women or women with dysplasia,” said Dr. Laniewski, referring to abnormal cell growth on the lining of the cervix or endocervical canal — the pathway from inside the uterus to the vagina. “Intriguingly, we also found that women with genital inflammation, or unhealthy vaginal bacteria, also have elevated specific immune checkpoints, suggesting these features of the local microenvironment also might contribute to cancer progression.”
“In addition to the promising evidence that reveals new biomarkers, this study highlights the potential utility of CVL profiling for predicting and monitoring response to therapy,” Dr. Herbst-Kralovetz said. “For the individual, a CVL is minimally invasive and even easier than a blood draw. This also could evolve into a self-collected sample, like a swab.”
These findings, combined with previous and other ongoing studies, provide a foundation for future studies for Dr. Herbst-Kralovetz and her research team. They intend to further study immune checkpoints to determine if, in addition to being a tool for early detection, they can be used to monitor and predict responses to cancer therapy.
“I’m incredibly passionate about creating interdisciplinary research teams to build our understanding of gynecologic cancers and the local microenvironment to positively impact women’s health outcomes,” Dr. Herbst-Kralovetz said. “This is a first step for precision medicine approaches for novel diagnostics, and it also may be a way for us to track how patients are responding to treatment.”
Story By: Blair Willis, communications specialist at the University of Arizona Cancer Center.
About the College
Founded in 2007, the University of Arizona College of Medicine – Phoenix inspires and trains exemplary physicians, scientists and leaders to advance its core missions in education, research, clinical care and service to communities across Arizona. The college’s strength lies in our collaborations and partnerships with clinical affiliates, community organizations and industry sponsors. With our primary affiliate, Banner Health, we are recognized as the premier academic medical center in Phoenix. As an anchor institution of the Phoenix Bioscience Core, the college is home to signature research programs in neurosciences, cardiopulmonary diseases, immunology, informatics and metabolism. These focus areas uniquely position us to drive biomedical research and bolster economic development in the region.
As an urban institution with strong roots in rural and tribal health, the college has graduated more than 1,000 physicians and matriculates 130 students each year. Greater than 60% of matriculating students are from Arizona and many continue training at our GME sponsored residency programs, ultimately pursuing local academic and community-based opportunities. While our traditional four-year program continues to thrive, we will launch our recently approved accelerated three-year medical student curriculum with exclusive focus on primary care. This program is designed to further enhance workforce retention needs across Arizona.
The college has embarked on our strategic plan for 2025 to 2030. Learn more.