Researchers Confirm Link Between Cancer Therapeutic and Cardiovascular Complications
Ponatinib has revolutionized the treatment of chronic myelogenous leukemia (CML) with the T315I mutation, leading to a significant impact on overall survival and prognosis. Unfortunately, the therapeutic has also been linked to cardiomyopathy, heart failure and vascular occlusion in a small percentage of patients.
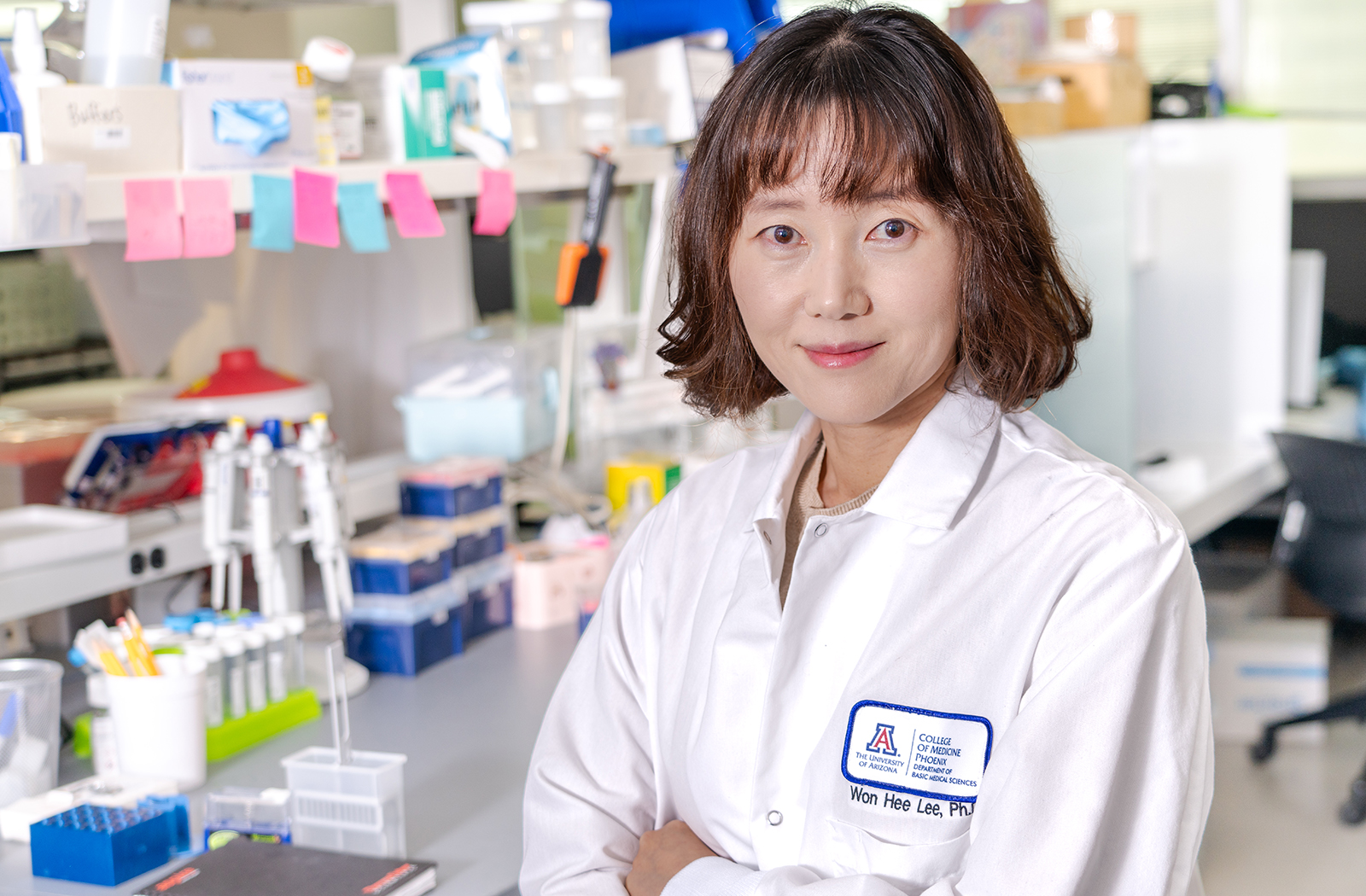
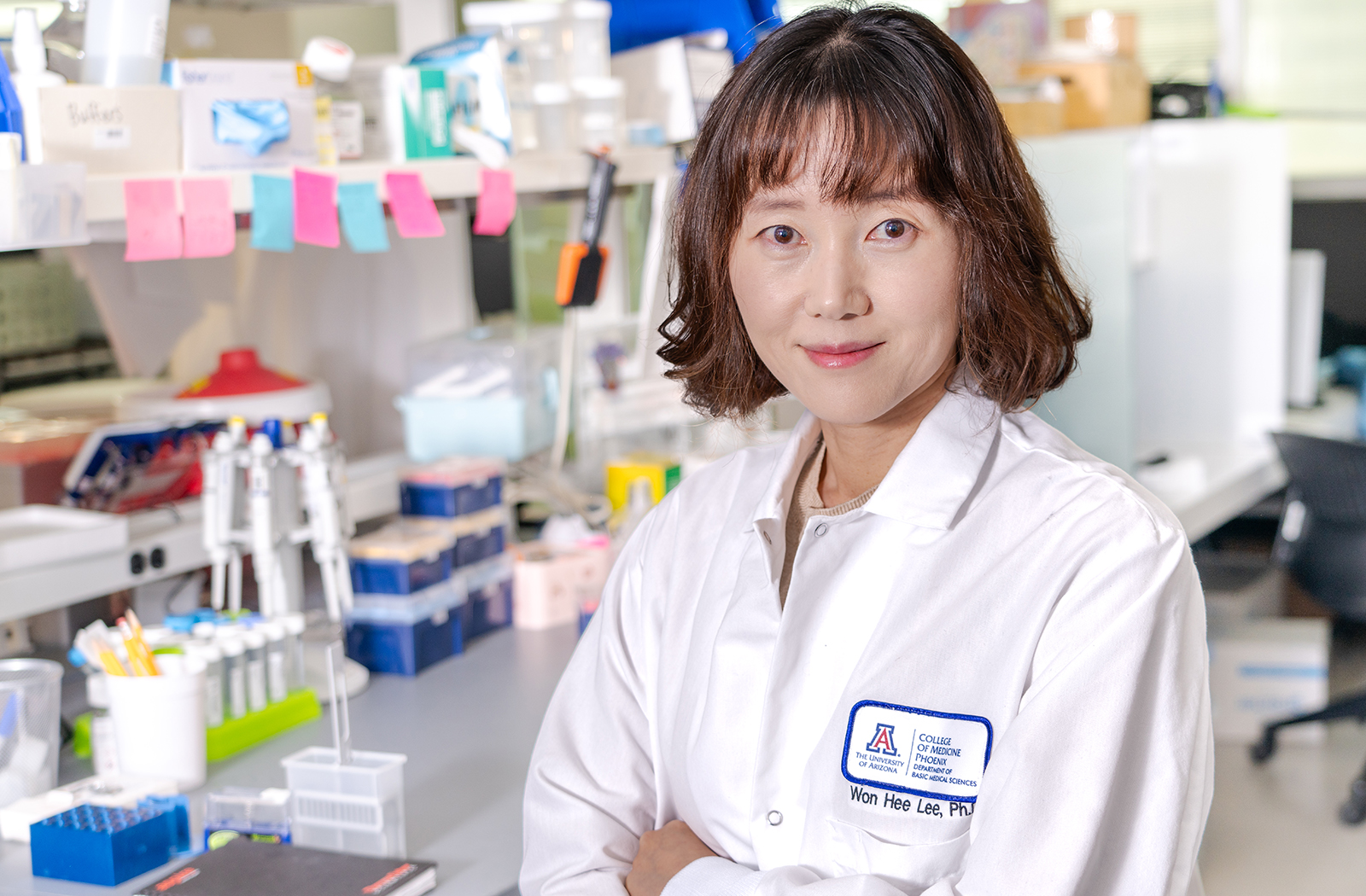
Won Hee Lee, PhD, assistant professor of Basic Medical Sciences at the University of Arizona College of Medicine – Phoenix, co-led a multi-institution study that examined this link. Their research — The Integrated Stress Response Potentiates Ponatinib-Induced Cardiotoxicity — was recently published in Circulation Research. It sought to correlate the reported ill effects of the drug on the heart.
“Since ponatinib is the sole option for CML patients with the T315I mutation, it is crucial to better understand the molecular mechanisms of ponatinib-induced cardiotoxicity and develop strategies to mitigate its adverse cardiotoxic effects,” Dr. Lee said.
Using human induced pluripotent stem cells-derived cardiomyocytes (iPSC-CMs), and a model, she, along with her fellow researchers, investigated the relationship between ponatinib-induced mitochondrial stress and the integrated stress response (ISR) and their role in promoting ponatinib-induced cardiotoxicity.
First, they had to demonstrate that ponatinib was in fact connected to increased cardiotoxicity. Treating three healthy hiPSC-CMs with ponatinib, their trials showed a dose-dependent decrease in cell viability.
Ponatinib also induced significant DNA double-strand breaks; and, through hi-speed video microscopy with motion vector analysis, they discovered a marked decrease in the velocity and frequency of contraction of ponatinib-treated hiPSC-CMs. “These data confirm the role of ponatinib treatment in cardiotoxicity and hiPSC-CMs’ impaired function and serves as a valid platform to investigate the pathophysiology underlying ponatinib-induced cardiotoxicity,” Dr. Lee explained.
So, with the link firmly established, their research aims shifted to identifying the signaling pathways that explain ponatinib-induced cardiotoxicity, as well as to further assessing how the integrated stress response inhibitor (ISRIB) can offer cardio protection against the effects of the drug.
These additional discoveries are fundamental to ensuring CML patients can get the care they need because without greater context, they are stuck in a medical bind. “In this situation, you have to decide which is more beneficial. Is it the higher risk or the higher benefits? That is why we are focused on finding that mechanism. Hopefully, we can use this inhibitor, so we have some great protections for these patients on their dose of treatment,” Dr. Lee said.
To carry on the investigation into the novel molecular mechanisms responsible for ponatinib-induced cardiotoxicity, Dr. Lee was recently awarded a grant from the National Institutes of Health (NIH). The grant extends to assessing whether a small-molecule ISRIB can mitigate the undesirable outcomes of ISR activation on the heart without compromising the efficacy of ponatinib on CML.
She hopes to ensure that patients using ponatinib can feel safe knowing their cancer can be treated without hesitation because their heart is protected.
Research reported in this story was supported by the NIH under project number 1R01HL164729-01A1.
The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
About the College
Founded in 2007, the University of Arizona College of Medicine – Phoenix inspires and trains exemplary physicians, scientists and leaders to advance its core missions in education, research, clinical care and service to communities across Arizona. The college’s strength lies in our collaborations and partnerships with clinical affiliates, community organizations and industry sponsors. With our primary affiliate, Banner Health, we are recognized as the premier academic medical center in Phoenix. As an anchor institution of the Phoenix Bioscience Core, the college is home to signature research programs in neurosciences, cardiopulmonary diseases, immunology, informatics and metabolism. These focus areas uniquely position us to drive biomedical research and bolster economic development in the region.
As an urban institution with strong roots in rural and tribal health, the college has graduated more than 1,000 physicians and matriculates 130 students each year. Greater than 60% of matriculating students are from Arizona and many continue training at our GME sponsored residency programs, ultimately pursuing local academic and community-based opportunities. While our traditional four-year program continues to thrive, we will launch our recently approved accelerated three-year medical student curriculum with exclusive focus on primary care. This program is designed to further enhance workforce retention needs across Arizona.
The college has embarked on our strategic plan for 2025 to 2030. Learn more.