Researchers Examining Key Connection Between Signaling Protein and Alzheimer’s
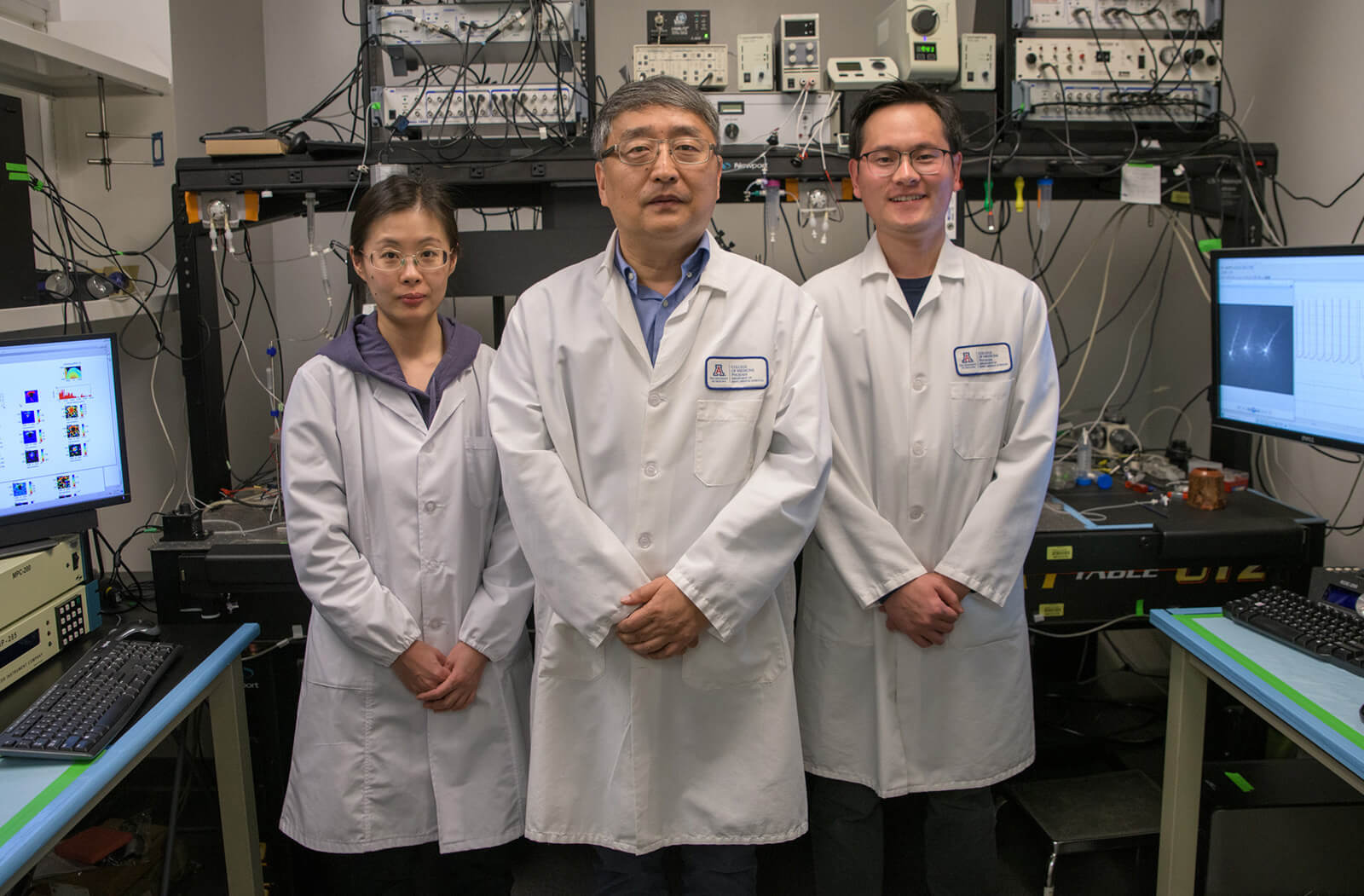
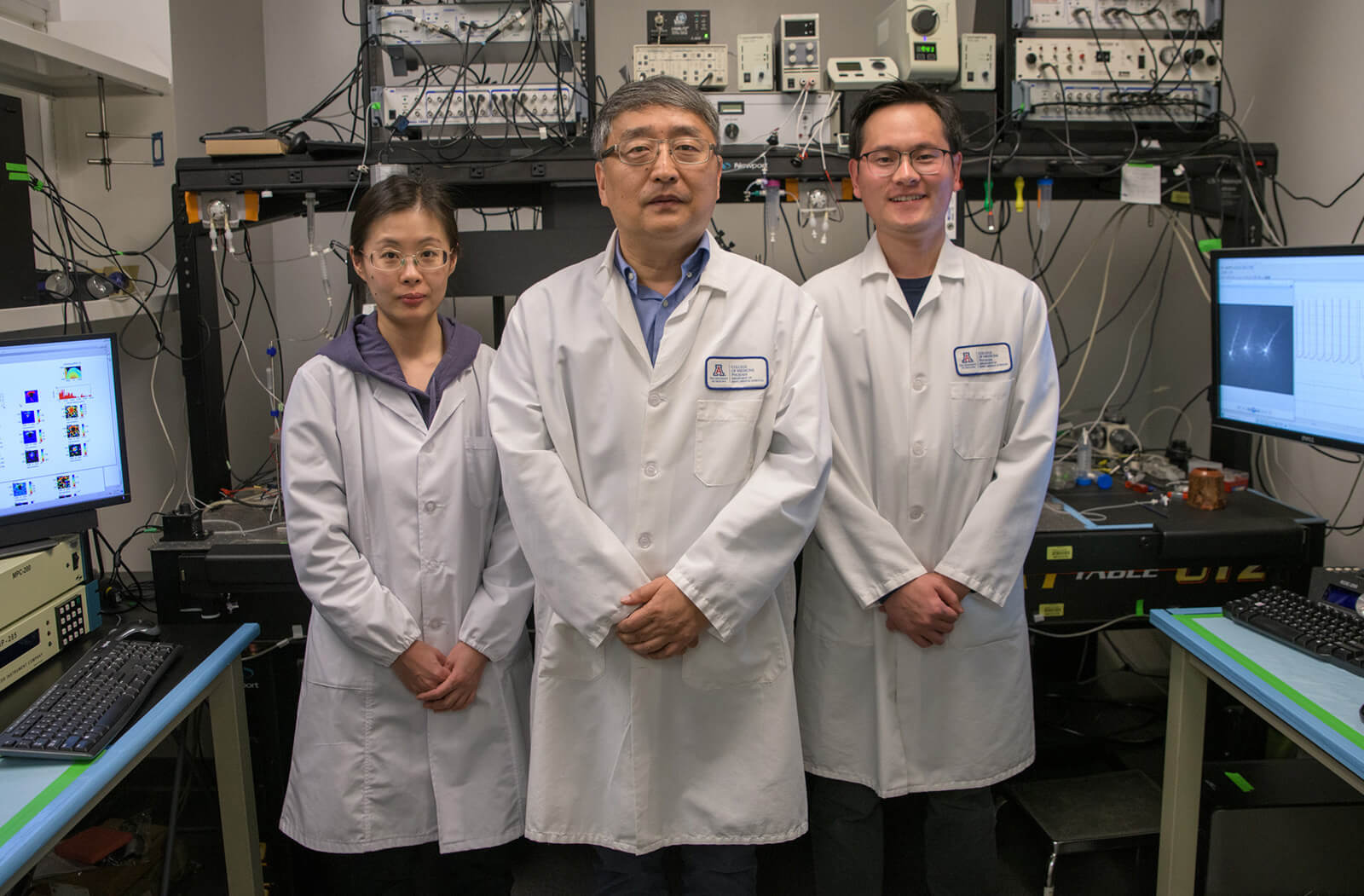
Researchers at the University of Arizona College of Medicine – Phoenix have identified that a reduction in the Mesenchymal Epithelial Transition (MET) protein in the brain may contribute to the risk an aging has of developing neurodegenerative disorders like Alzheimer’s disease (AD).
His laboratory has studied the role of the MET protein, which has been identified as a risk factor in the developing embryonic brain for autism. “One focus we have is on an autism risk gene called MET; together, with its signaling ligand, hepatocyte growth factor (HGF), it forms a critical signaling system during brain development” he said.
The MET protein’s signaling promotes neuronal survival, generates new connectivity and enhances plasticity — all characteristics of a young, healthy brain state. It was in those characteristics that Dr. Qiu made an interesting discovery.
Just as the role of MET can affect the developing brain, it may play a role in brain aging and degeneration. In fact, clinical literature has shown that the brains of AD patients have lower levels of the MET protein and HGF.
“More than 6 million Americans are currently living with AD. This is the disease that cost the U.S. economy an estimated $320 billion in 2022 — in addition to an estimated $271 billion in unpaid caregiving,” Dr. Qiu said.
The Centers for Disease Control forecasts the number will reach 14 million people by 2060. Every five years, the number of people over the age of 65 diagnosed with AD doubles. There are currently no effective treatments for AD.
“Our previous work has shown the neuroprotective, regenerating potential of HGF/MET, so our hypothesis is that enhancing the HGF/MET signaling should have beneficial effects in antagonizing aging and neurodegeneration and enhancing neural plasticity,” he explained.

“The success of this study may reveal a critical drug target for AD treatment, which may delay its onset, slow its progression, alleviate the brain’s pathological changes and improve cognition, as well as quality of life for AD patients.”
That potential impact has led Dr. Qiu to submit a proposal for a longer-term grant from the NIH, an R01. With further funding and a lengthened timeframe to conduct the research, Dr. Qiu and his team would have a greater opportunity to examine its potential beneficial effects.
Research reported in this story was supported by the NIH and National Institute of Aging under award number R21AG078700.
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
About the College
Founded in 2007, the University of Arizona College of Medicine – Phoenix inspires and trains exemplary physicians, scientists and leaders to advance its core missions in education, research, clinical care and service to communities across Arizona. The college’s strength lies in our collaborations and partnerships with clinical affiliates, community organizations and industry sponsors. With our primary affiliate, Banner Health, we are recognized as the premier academic medical center in Phoenix. As an anchor institution of the Phoenix Bioscience Core, the college is home to signature research programs in neurosciences, cardiopulmonary diseases, immunology, informatics and metabolism. These focus areas uniquely position us to drive biomedical research and bolster economic development in the region.
As an urban institution with strong roots in rural and tribal health, the college has graduated more than 1,000 physicians and matriculates 130 students each year. Greater than 60% of matriculating students are from Arizona and many continue training at our GME sponsored residency programs, ultimately pursuing local academic and community-based opportunities. While our traditional four-year program continues to thrive, we will launch our recently approved accelerated three-year medical student curriculum with exclusive focus on primary care. This program is designed to further enhance workforce retention needs across Arizona.
The college has embarked on our strategic plan for 2025 to 2030. Learn more.