
What is ABSITE?
ABSITE is an annual exam — 250 multiple-choice question, five-hours — that is offered by the American Board of Surgery. It primary objective is the testing of surgical knowledge. Its content is aligned with the SCORE Curriculum Outline for General Surgery Residency (PDF).
Additional Details:
- Testing takes place during the final two weeks of January, and results are provided by early March.
- The same exam is provided to all residents; however, percentile score is generated by comparing the raw score to your peers within the same PGY level.
- A sample test of the format is available for review.
Why is It Important?
The ABSITE reflects how well you are learning the requisite information needed to become a safe and successful general surgeon and serves as a component of your performance evaluation in the Clinical Competency Committee. That committee meets twice every year, and your performance on the exam may affect your PGY advancement. In addition, the text is a strong predictor for passing the General Surgery Qualifying Examination and may also be used by fellowships when evaluating residents for positions.
Study Strategies
- Develop a structured reading program for the entire year — daily or weekly — and stick to it. This may include:
- Textbook, the This Week in SCORE weekly topic, etc.
- Use a mixture of general topics with current rotation specific topics.
- The preparation for Thursday morning didactics.
- Create flashcards for high yield topics and topics that you find difficult to master.
- Utilize question banks to test yourself, increasing the number of questions as ABSITE gets closer.
- ACS Tips.
Resources
- SCORE:
- This Week in SCORE — weekly topics with associated reading, modules and quizzes.
- Question bank.
- Videos.
- Review Books:
- Podcasts:
- Question Banks:
- SCORE.
- TrueLearn.
Supporting Literature
- Flentje AO, Caturegli I, Kavic SM. Practice Makes Perfect: Introducing a Question Bank for ABSITE Preparation Improves Program Performance. J Surg Educ. 2020 Jan-Feb;77(1):54-60. doi: 10.1016/j.jsurg.2019.09.005. Epub 2019 Sep 14. PMID: 31526642.
- Qbanks improved overall ABSITE scores with more questions answered leading to larger improvement — three percent for every 100 questions completed.
- Qbanks improved overall ABSITE scores with more questions answered leading to larger improvement — three percent for every 100 questions completed.
- Winer LK, Cortez AR, Kassam AF, Quillin RC, Goodman MD, Makley AT, Sussman JJ, Kuethe JW. The Impact of a Comprehensive Resident Curriculum and Required Participation in "This Week in SCORE" on General Surgery ABSITE Performance and Well-Being. J Surg Educ. 2019 Nov-Dec;76(6):e102-e109. doi: 10.1016/j.jsurg.2019.08.015. Epub 2019 Sep 3. PMID: 31492638.
- Required “This week in SCORE” participation lead to increased weekly study time and median ABSITE percentile improvement of 12 percent.
- Required “This week in SCORE” participation lead to increased weekly study time and median ABSITE percentile improvement of 12 percent.
- de Virgilio C, Chan T, Kaji A, Miller K. Weekly Assigned Reading and Examinations during Residency, ABSITE Performance and Improved Pass Rates on the American Board of Surgery Examinations. J Surg Educ. 2008 Nov-Dec;65(6):499-503. doi: 10.1016/j.jsurg.2008.05.007. PMID: 19059184.
- Weekly assigned readings and quizzes resulting in increased first time ABS Qualifying Exam pass rates.
- ABSITE score less than the 30th percentile at any time or scoring less than 35th percentile more than once during residency significantly increased the chance of failing the ABS Qualifying Exam.
- ABSITE score less than the 25th percentile also predicted failure of both the ABS Qualifying and Certifying Exams.
- Kim JJ, Kim DY, Kaji AH, Gifford ED, Reid C, Sidwell RA, Reeves ME, Hartranft TH, Inaba K, Jarman BT, Are C, Galante JM, Amersi F, Smith BR, Melcher ML, Nelson MT, Donahue T, Jacobsen G, Arnell TD, de Virgilio C. Reading Habits of General Surgery Residents and Association With American Board of Surgery In-Training Examination Performance. JAMA Surg. 2015 Sep;150(9):882-9. doi: 10.1001/jamasurg.2015.1698. PMID: 26176352.
- Resident attitude regarding the importance of ABSITE results was among the independent predictors of ABSITE performance.
- Resident attitude regarding the importance of ABSITE results was among the independent predictors of ABSITE performance.
- Kim RH, Tan TW. Interventions that Affect Resident Performance on the American Board of Surgery In-Training Examination: A Systematic Review. J Surg Educ. 2015 May-Jun;72(3):418-29. doi: 10.1016/j.jsurg.2014.09.012. Epub 2014 Oct 31. PMID: 25456409.
- Systematic review of 26 published articles concluding that structured reading programs and mandatory remedial programs were the consistently most effective measure that can improve ABSITE performance.
- Systematic review of 26 published articles concluding that structured reading programs and mandatory remedial programs were the consistently most effective measure that can improve ABSITE performance.
- Miller AT, Swain GW, Widmar M, Divino CM. How Important are American Board of Surgery In-Training Examination Scores When Applying for Fellowships? J Surg Educ. 2010 May-Jun;67(3):149-51. doi: 10.1016/j.jsurg.2010.02.007. PMID: 20630424.
- Surgical fellowship directors ranked importance of ABSITE scores as three- or four- out of five-point scale.
- Only factors given more weight than ABSITE scores were letters of recommendation and candidate’s residency program.
- To be most competitive, applicants should aim to score >50th percentile.
- Marcadis AR, Spencer T, Sleeman D, Velazquez OC, Lew JI. Better ABSITE Performance with Increased Operative Case Load during Surgical Residency. Surgery. 2018 Dec;164(6):1341-1346. doi: 10.1016/j.surg.2018.06.004. Epub 2018 Jul 29. PMID: 30068483.
- Residents who perform more operative cases do better on ABSITE.
Included are a list of key studies (PDF) the faculty for each service have identified for residents to be familiar with prior to starting the rotation.
Supporting Resources
- American College of Surgeons (ACS) Risk Calculator – Estimates chances of morbidity/mortality of specific surgeries utilizing NSQIP data.
- Eastern Association for the Surgery of Trauma (EAST) – Practice management guidelines.
- Infectious Diseases Society of America (IDSA) – Clinical practice guidelines for treatment of infections.
- National Comprehensive Cancer Network (NCCN) – Comprehensive, up-to-date guidelines and management practices for cancers.
- PubMed – National library of medicine database.
- Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) – Large repository of surgical videos, images, webinars, virtual hernia clinic for preparation of laparoscopic/robotic cases.
- Surgical Council on Resident Education (SCORE) – General surgery resident curriculum portal.
- SurgicalCriticalCare.net – ICU resource with evidence-based guidelines, calculators, lectures and videos.
- University of Arizona Medical Library – Access textbooks, publications and more.
- Western Trauma Association (WTA) – Trauma algorithms.
Textbooks
The following textbooks are available through University of Arizona Medical Library:
- Sabiston Textbook of Surgery: The Biological Basis of Modern Surgical Practice.
- Greenfield's Surgery: Scientific Principles and Practice.
- Schwartz’s Principles of Surgery.
- Fischer’s Mastery of Surgery.
- Cameron’s Surgical Therapy.
- Zollinger’s Atlas of Surgical Operations.
- Marino’s The ICU Book.
- Operative Techniques in Surgery.
- Clinical Scenarios in Surgery.
- Operative Dictations in General and Vascular Surgery.
- Vascular Surgery for the General Surgeon.
- Clinical Algorithms in General Surgery.
Program and Time Requirements
- A minimum of five years of progressive residency education.
- Sixty months of training at no more than three residency programs.
- At least 48 weeks of full clinical activity in each residency year.
- Can be averaged over first three years of residency — for total of 144 weeks required.
- Can be averaged over last two years of residency — for total of 96 weeks required.
- At least 54 months of clinical surgical experience with no more than six months assigned to non-clinical or non-surgical disciplines.
- Final two years of residency — PGY4 and PGY5 — in the same program.
Specific Requirements
- Advanced Cardiovascular Life Support (ACLS).
- Advanced Trauma Life Support (ATLS).
- Fundamentals of Laparoscopic Surgery (FLS).
- Fundamentals of Endoscopic Surgery (FES).
- Complete at least six operative and six clinical performance assessments — generally completed in the PGY5 year.
- Clinical Assessment and Management Exam (CAMEO).
- Operative Performance Rating System (OPRS).
- Choose from: Appendectomy, cholecystectomy, colectomy, small bowel resection, inguinal hernia repair, ventral hernia repair, AV fistula creation, lumpectomy with axillary management, thyroidectomy and parathyroidectomy.
Chief Resident Year
- Act in the capacity of chief resident for a minimum of 48 weeks over PGY4 and PGY5 years.
- Finish the entire chief resident experience in either the content areas of general surgery or thoracic surgery with no more than four months devoted to any one area.
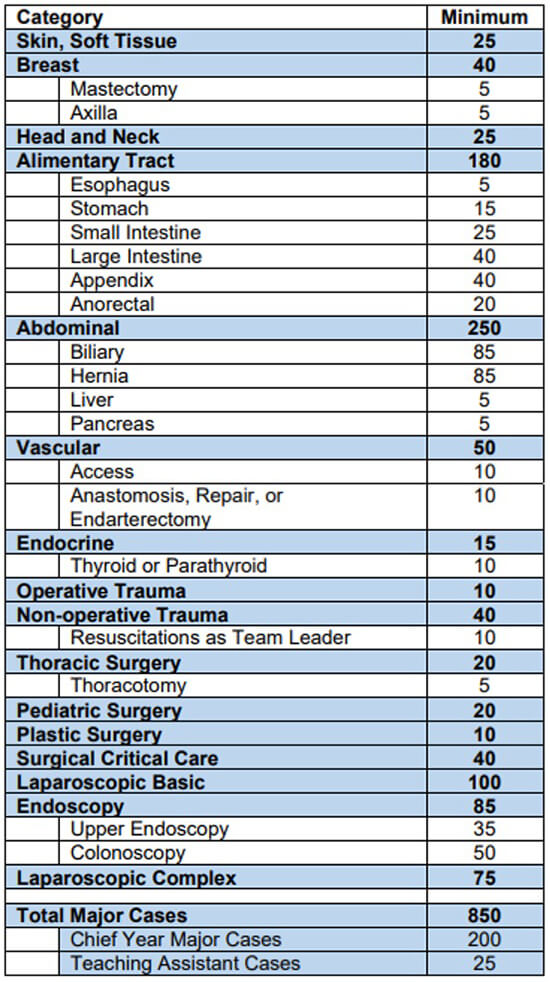
Operative Requirements
- At least 850 total operative procedures over five years.
- At least 250 operative procedures — as a surgeon junior or first assist — by the end of the PGY2 year with only up to 50 in non-defined categories counting toward the total.
- At least 200 operative procedures in the chief resident year.
- At least 25 cases as a teaching assistant.
- These do not count toward the 200 chief resident year cases.
- At least 40 cases in surgical critical care with at least one in each of the following seven categories (each case entered must have two or more of the categories logged):
- Ventilator management.
- Bleeding.
- Hemodynamic instability.
- Organ dysfunction/failure.
- Dysrhythmias.
- Invasive line management/monitoring.
- Parenteral/enteral nutrition.
More details from ABS.
ACGME Case Log Instructions
- Only one resident can take credit for each operation as Surgeon Junior/Surgeon Chief.
- Exception: Vascular exposures – One resident can log the exposure by adding “E” before the case ID and another resident can log anastomosis/repair.
- If a senior resident takes credit for the case, a junior resident can log case as First Assistant.
- Alternatively, if a senior resident takes credit as the Teaching Assistant, then a junior resident can log as Surgeon Junior.
- Log all procedures you perform in the case; however, you will only be able to take credit for one that will be applied to your case log minimums.
- Check the box in the upper right corner for any cases that involve trauma.
- Change the patient type to Pediatric to log pediatric cases for any patient <13-years-old.
- This ensures the cases count toward your pediatric minimum — even for cases that do not have specific pediatric codes.
- For robotic cases, log them as Laparoscopic and in the comments write Robotic.
Roles
- Surgeon Chief – PGY5 when operating as the primary surgeon.
- Surgeon Junior – PGY1 to PGY4 when operating as the primary surgeon.
- First Assistant – Any case in which a resident assists with an operation when an attending or more senior resident is performing the operation as the primary surgeon.
- Teaching Assistant – PGY4 to PGY5 senior resident taking a junior resident through a case.
ACGME Case Log Minimums
Procedure Case Codes
The attached ACGME case codes (PDF) are not meant to be a complete list, but should cover the vast majority of cases you may perform during the general surgery residency.
- Clinical and educational work hours must be limited to no more than 80 hours per week, averaged over a four-week period, inclusive of all in-house clinical and educational activities, clinical work done from home and all *moonlighting.
- Preparing for following day’s cases, studying and research do not count toward the 80 hours.
- Residents should have eight hours off between scheduled clinical work and education periods.
- Residents must have at least 14 hours free of clinical work and education after 24 hours of in-house call.
- Residents must be scheduled for a minimum of one day in seven that is free of clinical work and required education when averaged over four weeks.
- At-home call cannot be assigned on these free days.
- Clinical and educational work periods for residents must not exceed 24 hours of continuous scheduled clinical assignments.
- Up to four hours of additional time may be used for activities related to patient safety — such as providing effective transitions of care — and/or resident education.
- Additional patient care responsibilities must not be assigned to a resident during this time.
- In rare circumstances — after handing off all other responsibilities — a resident, on their own initiative, may elect to remain or return to the clinical site in the following circumstances:
- To provide care to a single severely ill or unstable patient.
- To give humanistic attention to the needs of a patient or family.
- To attend unique educational events.
- These additional hours of care or education will be counted toward the 80-hour weekly limit
- Night float must occur within the context of the 80-hour and one day-off-in-seven requirements.
- Night float rotations must not exceed two months in duration, four months of night float per PGY level and 12 months for the entire program.
- Residents must be scheduled for in-house call no more frequently than every third night when averaged over a four-week period.
- Time spent on patient care activities by residents on at-home call must count toward the 80-hour maximum weekly limit. The frequency of at-home call is not subject to the every third-night limitation, but must satisfy the requirement for the one day in seven free of clinical work and education when averaged over four weeks.
- Residents are permitted to return to the hospital while on at-home call to provide direct care for new or established patients. These hours of inpatient patient care must be included in the 80-hour maximum weekly limit.
*Moonlighting Policy: Moonlighting is prohibited. No exceptions.
Our residents have access to their own companion resource website. Banner-affiliated login credentials are needed to access this resource.