Researchers Seeking to Understand if Traumatic Brain Injury can Alter the Gut Microbiota
Researchers at the University of Arizona College of Medicine – Phoenix are seeking to understand if traumatic brain injury (TBI) can cause chronic changes in the gut microbiota and the impact of the microbiome on post-concussive symptoms.
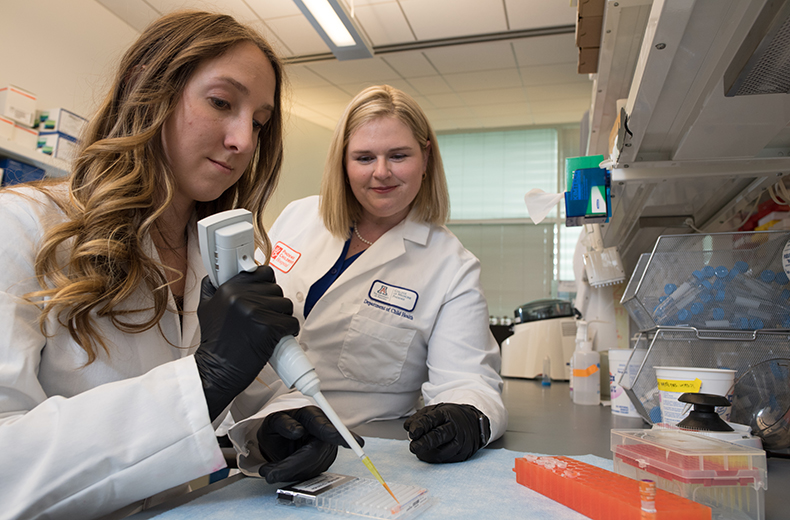
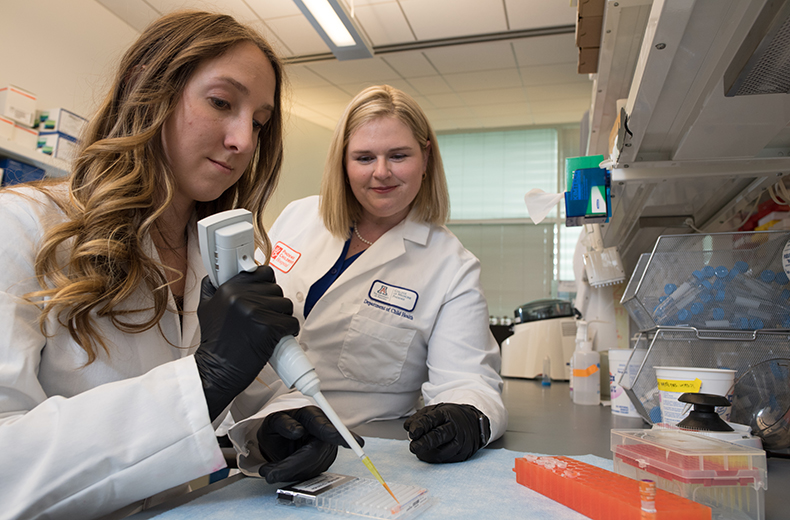
Theresa Thomas, PhD, an assistant professor, and Gokul Krishna, PhD, a postdoctoral research associate, in the Translational Neurotrauma Research Program at the University of Arizona College of Medicine – Phoenix and Barrow Neurological Institute at Phoenix Children’s Hospital, were awarded $10,000 by the Valley Research Partnership to further research in TBIs.
Dr. Thomas discussed their latest research.
Explain Your Research
More than 50 percent of TBI survivors suffer from post-concussive cognitive, emotional and sensory symptoms that endure for months to years post-injury. These symptoms are caused by altered communication within the brain. Recent research indicates that this communication can be influenced, in part, by interactions between the brain and the gut through molecules produced from bacterial flora (microbiota), which can change in response to antibiotics, diet, stress or other external factors.
We are seeking to identify if a traumatic brain injury can cause acute and chronic imbalances in the gut microbiota that could contribute to persisting post-concussive symptoms.
Why is This Important?

What was Your Motivation for Studying TBI and Gut Health?
Studies show that several neurological deficits are driven or exacerbated by a disrupted microbial population. Inspired by these reports, our current interest is on how psychological processes are impacted when the bacterial status of the microbiota is influenced by traumatic brain injury. As scientific researchers, our goal is to identify the “mediators” of brain function, so we can more efficiently use resources to reduce the risk of long-term disability after TBI.
Why Now?
The development of post-traumatic symptoms is among the most prevalent condition after a traumatic brain injury and exacts a huge toll on the individual, their family and society. Currently, we do not have an effective strategy to lessen this burden. Growing evidence indicates that the collection of microorganisms (collectively termed microbiota) in the gastrointestinal tract can influence brain and behavior. With prior knowledge regarding acute changes in gut microbiota, our research will assess long-term changes in gut microbiota and assess its influence regarding development and persistence of these post-traumatic symptoms.
Our research also proposes to look at sex differences. In this way, we are on an exciting path just at its beginning to shed insights into the biological relationship of TBI with implications for management of post-traumatic problems.
Topics
About the College
Founded in 2007, the University of Arizona College of Medicine – Phoenix inspires and trains exemplary physicians, scientists and leaders to advance its core missions in education, research, clinical care and service to communities across Arizona. The college’s strength lies in our collaborations and partnerships with clinical affiliates, community organizations and industry sponsors. With our primary affiliate, Banner Health, we are recognized as the premier academic medical center in Phoenix. As an anchor institution of the Phoenix Bioscience Core, the college is home to signature research programs in neurosciences, cardiopulmonary diseases, immunology, informatics and metabolism. These focus areas uniquely position us to drive biomedical research and bolster economic development in the region.
As an urban institution with strong roots in rural and tribal health, the college has graduated more than 1,000 physicians and matriculates 130 students each year. Greater than 60% of matriculating students are from Arizona and many continue training at our GME sponsored residency programs, ultimately pursuing local academic and community-based opportunities. While our traditional four-year program continues to thrive, we will launch our recently approved accelerated three-year medical student curriculum with exclusive focus on primary care. This program is designed to further enhance workforce retention needs across Arizona.
The college has embarked on our strategic plan for 2025 to 2030. Learn more.