UA Professor Receives Grant for Innovative Research in Preventing Heart Failure
A University of Arizona College of Medicine – Phoenix researcher has received a $393,493 grant from the National Institutes of Health to further her research in reducing the risk of heart failure in patients with high blood pressure.
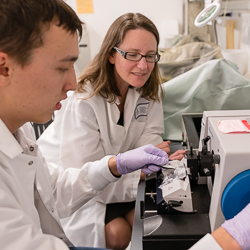
Fibroblasts are cells in connective tissue that produce collagen and play a critical role in healing. An over-production of collagen, also known as fibrosis, is a common end-stage characterization of nearly every type of heart disease. No approved therapy that directly targets the cells responsible for fibrosis exists. Utilizing ACE inhibitors, Dr. Hale hopes to find a way to kill off a small population of the fibroblasts responsible for the excessive fibrotic response to heart attack or to long-standing hypertension.
ACE inhibitors are a class of commonly used antihypertensive drugs that lower blood pressure by relaxing arteries and promoting excretion of salt and water. ACE inhibitors also have also been shown to protect the heart, in part by reducing collagen deposition.
“If we can identify subsets of cells that may appear with the development of hypertension, we can develop tools to directly target those cells, and prevent progression toward heart failure,” Dr. Hale said.
Medical advancements have allowed people to survive a heart attack, however, the damaged tissue eventually can lead to heart failure.
“Heart disease has been the No. 1 killer for decades,” Dr. Hale said. “In the last 10 years or so, we have more people surviving heart attacks which is great, but consequently, we have more people progressing to heart failure.”
After a heart attack, scar tissue forms to repair and replace the tissue that has been destroyed. This scar tissue impairs the cardiac contraction necessary to pump blood throughout the body. Over time, the scar tissue continues to expand beyond the initial site of injury in the heart. This can cause stiffening of the heart wall and eventually lead to heart failure.
Dr. Hale recognized that to slow the progression to heart failure, researchers needed to find the subpopulation of fibroblasts that may be responsible for the excess scar tissue.
“We need to do better, and right now with the drugs that we have on the market, we still see this progression to heart failure,” Dr. Hale said. “We need to find new treatment strategies to stop that course.”
Dr. Hale’s NIH grant is 1R56HL141165-01. More about her research.
About the College
Founded in 2007, the University of Arizona College of Medicine – Phoenix inspires and trains exemplary physicians, scientists and leaders to advance its core missions in education, research, clinical care and service to communities across Arizona. The college’s strength lies in our collaborations and partnerships with clinical affiliates, community organizations and industry sponsors. With our primary affiliate, Banner Health, we are recognized as the premier academic medical center in Phoenix. As an anchor institution of the Phoenix Bioscience Core, the college is home to signature research programs in neurosciences, cardiopulmonary diseases, immunology, informatics and metabolism. These focus areas uniquely position us to drive biomedical research and bolster economic development in the region.
As an urban institution with strong roots in rural and tribal health, the college has graduated more than 1,000 physicians and matriculates 130 students each year. Greater than 60% of matriculating students are from Arizona and many continue training at our GME sponsored residency programs, ultimately pursuing local academic and community-based opportunities. While our traditional four-year program continues to thrive, we will launch our recently approved accelerated three-year medical student curriculum with exclusive focus on primary care. This program is designed to further enhance workforce retention needs across Arizona.
The college has embarked on our strategic plan for 2025 to 2030. Learn more.