Access to Mental Health and PCP Appointments Fatigue Mitigation Psychological Safety Well-Being National Resources The ABCs of Psychological Safety
Program leaders are encouraged to use institutional and national tools, as well as the implementation ideas collated by the leadership of the University of Arizona College of Medicine – Phoenix GME programs and listed on these resource pages to support their improvement efforts.
Well-being 1: Access to Mental Health and PCP Appointments
| Level 1 | Level 2 | Level 3 | Level 4 | Level 5 |
|---|---|---|---|---|
| The program supports residents and fellows who request time off for personal/ family* medical and mental health appointments by following the Banner Health and GME policies. | The program has a written procedure shared with residents/fellows annually for residents/fellows to allow time off in advance for personal/immediate family medical and mental health appointments. | The program's residents/fellows and faculty can describe the procedures for requesting and accessing time off in advance for personal/immediate family medical and mental health appointments. The program has dedicated time in the schedule for all residents/fellows to attend to medical and mental health appointments at least several times a year. |
The program's residents/fellows actively apply and utilize the procedure for requesting and accessing time off in advance for personal/immediate family medical and mental health appointments. The program reminds and reinforces the value of residents/fellows utilizing their dedicated time in the schedule to attend to medical and mental health appointments at least several times a year. |
The program is an institutional and/or national model for policy, resources, education, and positive culture around providing time away for personal/immediate family medical and mental health appointments. Other programs look to your program for guidance and advice on this topic. |
💡Idea 1: Disseminate list of PCPs and dentists covered by Banner insurance at intern orientationTools:
|
💡Idea 2: Create relationship with specific office (Banner FM or IM) to schedule residents with faculty physicians.Tools: Implementation:
|
💡Idea 3: Create a pathway, well known to residents and fellows, that allows immediate time off when needed for personal/immediate family medical and mental health appointments.Tools:
|
Literature search |
Well-being 2: Fatigue Mitigation
| Level 1 | Level 2 | Level 3 | Level 4 | Level 5 |
|---|---|---|---|---|
| The program supports residents and fellows who request transition of care when maximally fatigued. All residents/fellows & faculty receive training to recognize the signs of fatigue and sleep deprivation, alertness management & fatigue mitigation processes. |
The program has a written procedure shared with residents/fellows annually that highlights resources and processes for getting assistance when house staff are maximally fatigued. | The program's residents/fellows and faculty can describe the procedures for identifying and supporting a resident/fellow who is maximally fatigued. | The program's faculty and residents/fellows are comfortable requesting and apply the procedure when maximally fatigued and utilize it. | The program is an institutional and/or national model for policy, resources, education, and positive culture around fatigue mitigation. Other programs look to your program for guidance and advice on this topic. |
💡Idea 1: Training to recognize the signs of fatigue and sleep deprivation, alertness management & fatigue mitigation processesTools:
|
💡Idea 2: Create a written procedure to highlight resources and processes for getting assistance when maximally fatigued (level 2)Tools:
|
Literature search |
Well-being 3: Psychological Safety
| Level 1 | Level 2 | Level 3 | Level 4 | Level 5 |
|---|---|---|---|---|
| The program is inclusive of all residents/fellows and keeps them from harm. It allows them to be themselves and accepts them for who they are, including their unique attributes and defining characteristics. | The program satisfies the needs of all residents/fellows to learn and grow. They feel safe to ask questions, give and receive feedback, try new things, and even make mistakes. | The program regularly engages residents/fellows to share ideas for improvement and incorporates these ideas in meaningful ways to improve the program. | The program welcomes challenging feedback provided by residents/fellows to make the program better. Residents/fellows feel safe to speak up and challenge the status quo. The program communicates progress on the desired opportunities to change or improve. | The program is an institutional and/or national model for policy, resources, education, and positive culture around improvement and gathering and receiving feedback. Others look to your program for guidance and advice on this topic. |
💡Idea 1: Program Leadership ApproachabilityTools:
|
💡Idea 2: Forums for Residents/Fellows to share ideas and where the program can welcome challenging feedback and demonstrate the actions being taken based on itTools:
|
💡Idea 3: Program flexibility and support for individualized goalsTools: |
Literature search |
The Leader's Tool Kit for Building Psychological Safety
| 1. Setting the Stage | 2. Inviting Participation | 3. Responding Productively | |
|---|---|---|---|
| Leadership Tasks: | Frame the Work
|
Demonstrate Situational Humility
|
Express Appreciation
|
| To Accomplish: | Shared expectations and meaning | Confidence that voice is welcome | Orientation toward continuous learning |
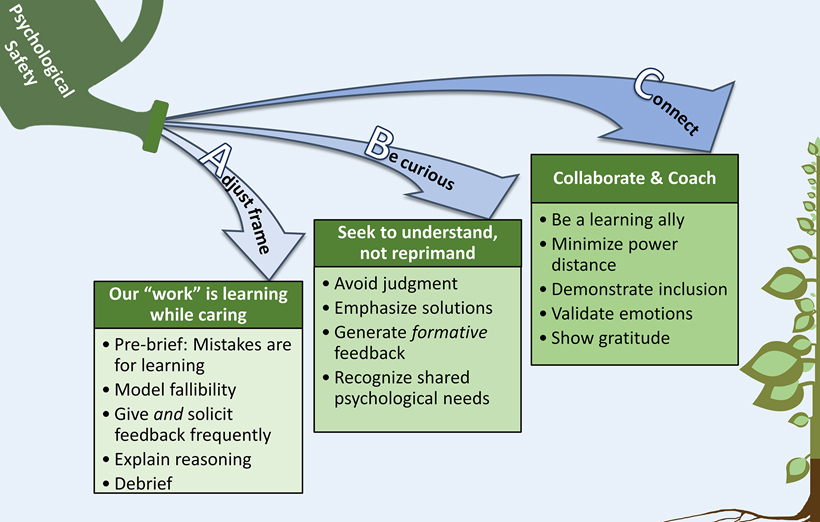
The ABCs of psychological safety
Well-Being National Resources (update quarterly)
- Compendium of Key Resources for Improving Clinician Well-Being - National Academy of Medicine (nam.edu)
- ACGME AWARE Well-being Course - Accreditation Council for Graduate Medical Education
- The ABCs of Cultivating Psychological Safety for Clinical Learner Growth
Do you have a well-being tool to share or need more help? Contact @email and Steven.Brown@bannerhealth.com