Breaking the Cycle of Liver Damage
A promising new therapy developed at the University of Arizona College of Medicine – Phoenix could transform the treatment of liver fibrosis by disrupting a key protein interaction that drives organ scarring.
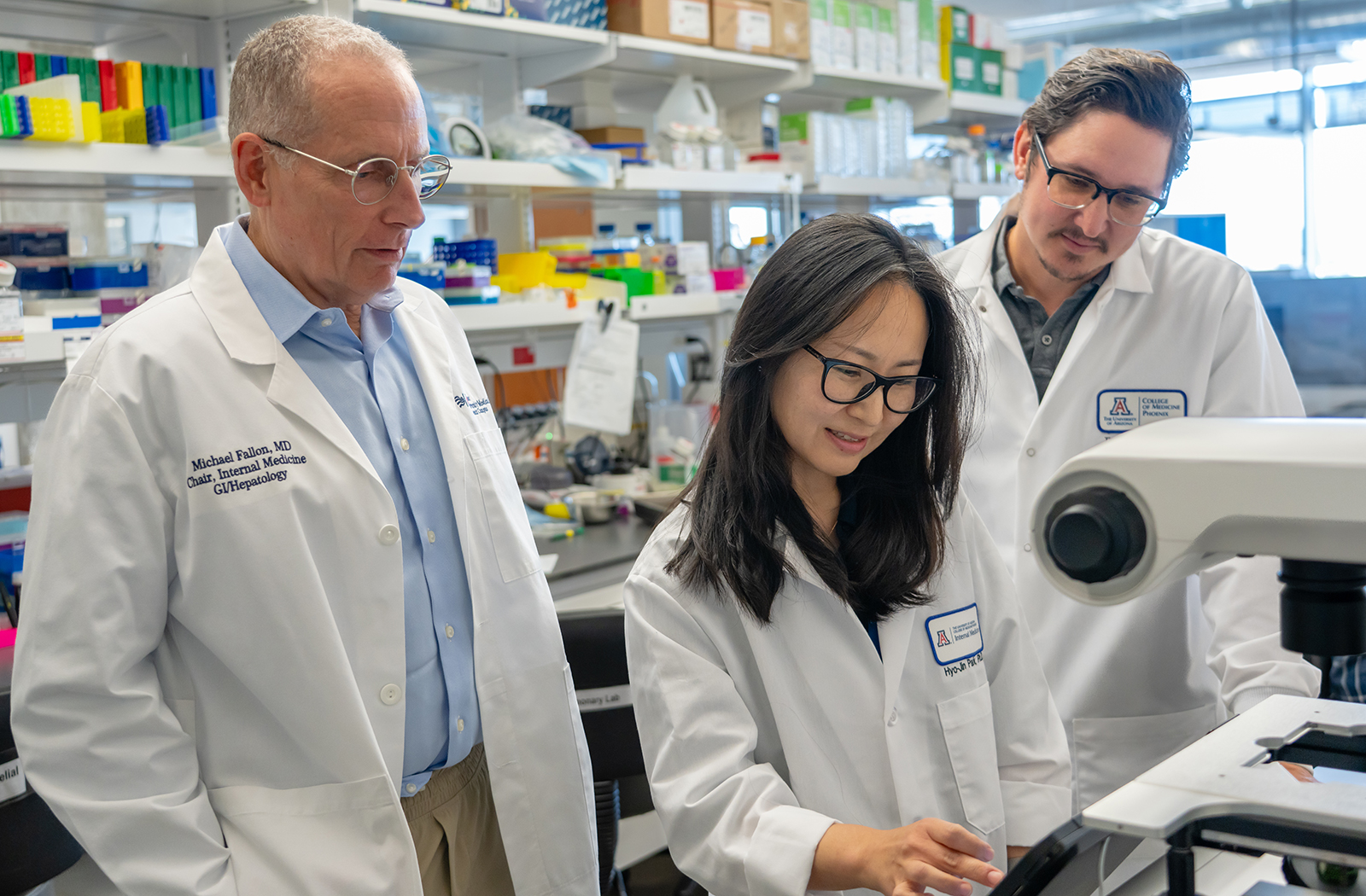
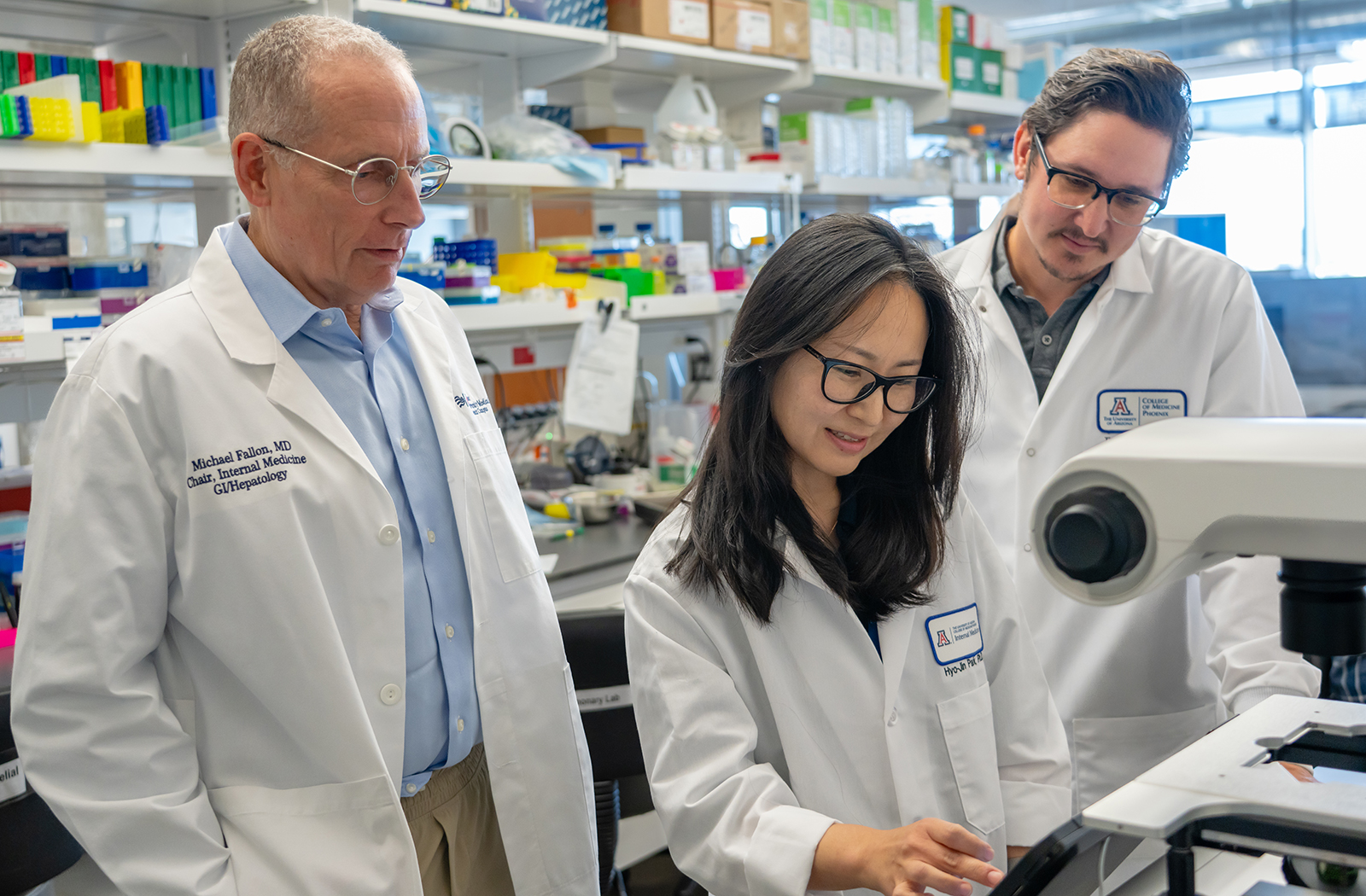
The project — co-led by Timothy Marlowe, PhD, associate professor in the Department of Internal Medicine, the U of A Cancer Center and the College of Pharmacy, Michael Fallon, MD, FACP, executive director for Clinical Research and chair of the Department of Internal Medicine, and Hyo Jin Park, PhD, assistant research scientist in the Department of Internal Medicine — targets the connection between focal adhesion kinase (FAK) and paxillin, two proteins that become hyperactive during fibrosis and fuel the buildup of scar tissue in the liver.

According to the Centers for Disease Control and Prevention (CDC), an estimated 4.5 million U.S. adults have been diagnosed with liver disease. This novel approach could represent a breakthrough for patients with metabolic-associated steatotic liver disease and alcohol-related liver disease, both of which currently have limited treatment options.
“We’re seeing a surge in patients with cirrhosis and liver cancer,” said Dr. Fallon. “The underlying issue in many of these cases is unchecked fibrosis. What we’re doing is targeting the root of that process.”
The team’s therapeutic candidate is a first-in-class peptide inhibitor, called FN-2012, designed to break the physical connection between paxillin and FAK within the cell’s focal adhesion complex — a structure that regulates cellular behavior and scar formation. “Think of paxillin and FAK as partners in a destructive feedback loop,” explained Dr. Marlowe. “By interrupting their interaction, we’re effectively collapsing the structural foundation that allows fibrosis to progress.”
Unlike traditional therapies that attempt to inhibit FAK’s enzymatic activity — often with poor specificity and side effects — FN-2012 works by disrupting protein-protein binding. This approach avoids the common pitfalls of small-molecule drugs that affect multiple targets in the body.
“Peptides are highly specific, biologically compatible and much less toxic,” Dr. Marlowe said. “So far, we’ve seen no toxicity in our preclinical studies.”
To improve stability and delivery, the researchers modified FN-2012 with a lipid tail to enhance its ability to penetrate cells. Early testing in models has shown a 45–50% reduction in liver fibrosis, with newer versions of the molecule aiming for over 60%.
“This type of precision design is only possible when you truly understand how these proteins interact at the molecular level,” said Dr. Park, who leads the molecular biology and imaging studies. “We used structural modeling and biophysical tools to confirm exactly how the peptide binds and blocks the interaction. This validation is crucial for moving toward clinical development.”
Dr. Park emphasized the translational potential of the therapy. “We’re already seeing signs that this strategy could be effective in multiple types of liver fibrosis,” she said. “And we’re continuing to refine the molecule for even better delivery and potency.”
“Our focus now is preparing for clinical trials,” said Dr. Fallon. “In Phase I, our main goals will be safety and proving the drug is hitting its target — the FAK-paxillin complex — in fibrotic liver tissue.” Though reversing fibrosis takes time, the researchers are also working to identify biomarkers of target engagement, which could accelerate clinical progress. An oral version of the drug is also in development to improve patient convenience.
This strategy could have broader implications, too. Since FAK and paxillin are also involved in cancer metastasis, future applications may extend beyond liver disease. “There’s a lot of potential here,” said Dr. Marlowe. “But for now, our priority is liver fibrosis, where the need for safe, effective therapies is urgent and growing.”
With liver disease affecting millions worldwide and few treatments currently available, this Arizona-based innovation may offer a much-needed new path forward.
If you’re interested in supporting liver fibrosis research, please contact Julie Bowe.
This research was supported by the National Institute of Diabetes and Digestive and Kidney Diseases under project number R42DK141379.
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Diabetes and Digestive and Kidney Diseases.
About the College
Founded in 2007, the University of Arizona College of Medicine – Phoenix inspires and trains exemplary physicians, scientists and leaders to advance its core missions in education, research, clinical care and service to communities across Arizona. The college’s strength lies in our collaborations and partnerships with clinical affiliates, community organizations and industry sponsors. With our primary affiliate, Banner Health, we are recognized as the premier academic medical center in Phoenix. As an anchor institution of the Phoenix Bioscience Core, the college is home to signature research programs in neurosciences, cardiopulmonary diseases, immunology, informatics and metabolism. These focus areas uniquely position us to drive biomedical research and bolster economic development in the region.
As an urban institution with strong roots in rural and tribal health, the college has graduated more than 1,000 physicians and matriculates 130 students each year. Greater than 60% of matriculating students are from Arizona and many continue training at our GME sponsored residency programs, ultimately pursuing local academic and community-based opportunities. While our traditional four-year program continues to thrive, we will launch our recently approved accelerated three-year medical student curriculum with exclusive focus on primary care. This program is designed to further enhance workforce retention needs across Arizona.
The college has embarked on our strategic plan for 2025 to 2030. Learn more.