The Classic ‘Chicken-or-Egg’ Question Comes to Cancer
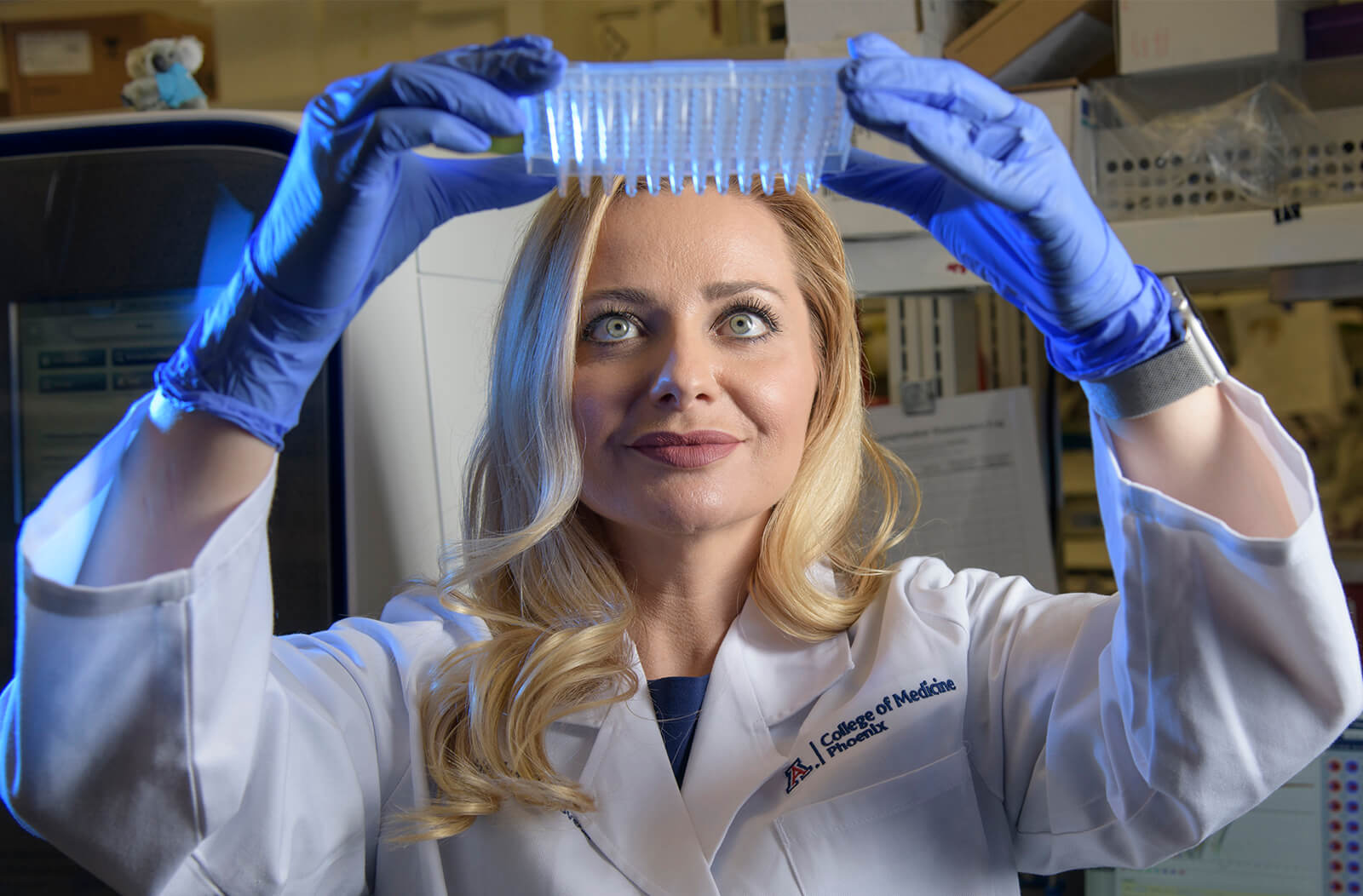
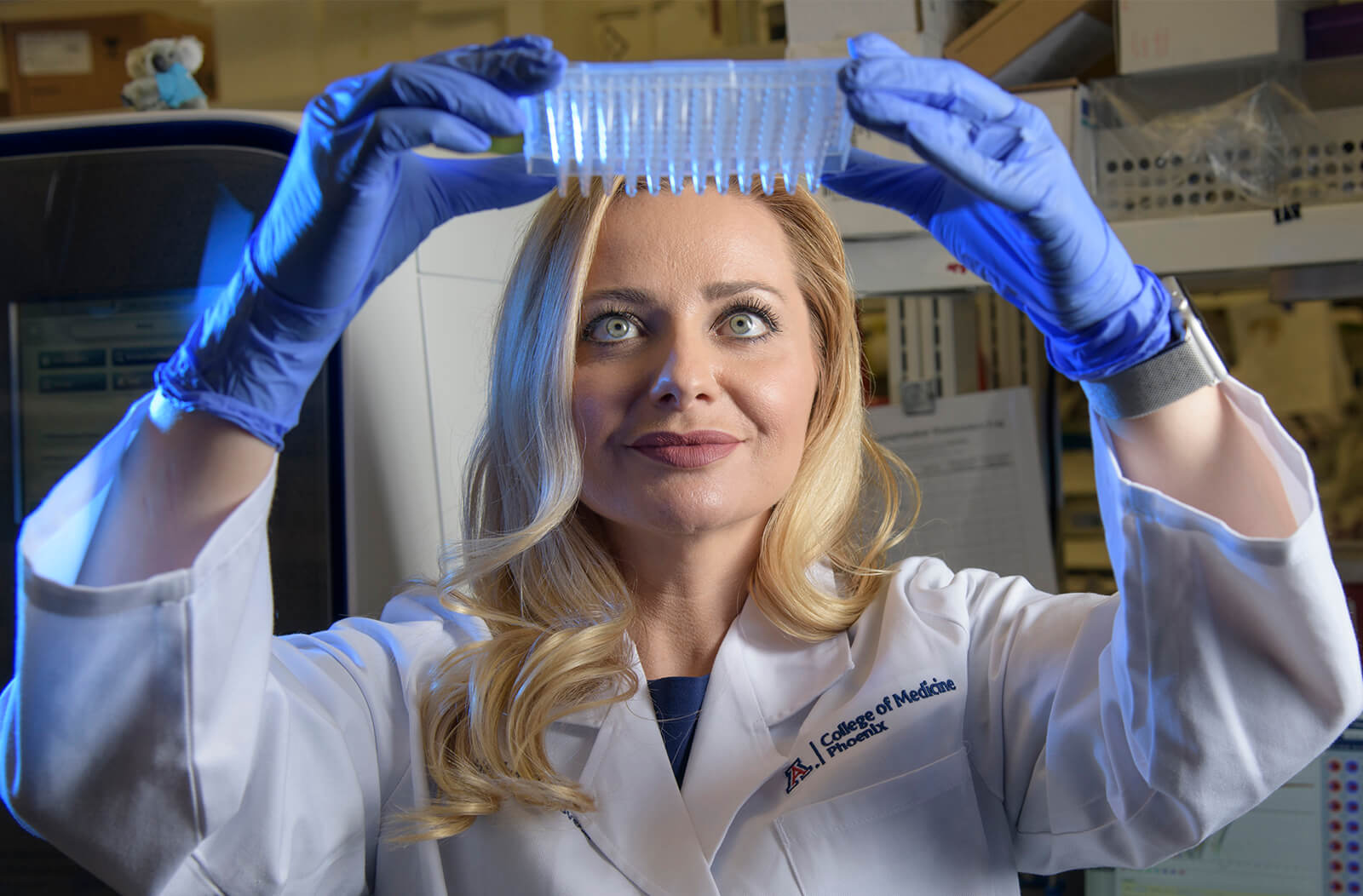
Unanswered questions swirl around the microbiome — habitats in our bodies that diverse species of bacteria call home. Scientists are only just starting to scratch the surface of how these bacteria interact with our unique body chemistries to influence our health. One of those scientists is Melissa Herbst-Kralovetz, PhD, associate professor of Basic Medical Sciences and Obstetrics/Gynecology at the University of Arizona College of Medicine – Phoenix, director of the Women’s Health Microbiome Initiative, and member of the U of A Cancer Center, who says the riddles posed by the vaginal microbiome captivated her early in her career.

Today, from her lab on the Phoenix Biomedical Campus in downtown Phoenix, Dr. Herbst-Kralovetz leads a team of researchers who are working to better understand how to predict, prevent and treat gynecologic cancers.
Bad Bugs and Gynecologic Cancer
One of the microbiome’s many mysteries involves the single-celled version of the eternal question: What came first, the chicken or the egg? In the Herbst-Kralovetz Lab, that question is more like: What came first, the cancer or the bugs? It’s a deceptively complex question, and the answer can tell us if we can prevent certain types of cancer or simply predict them — and gets to the heart of one of the most important concepts in science: causation.
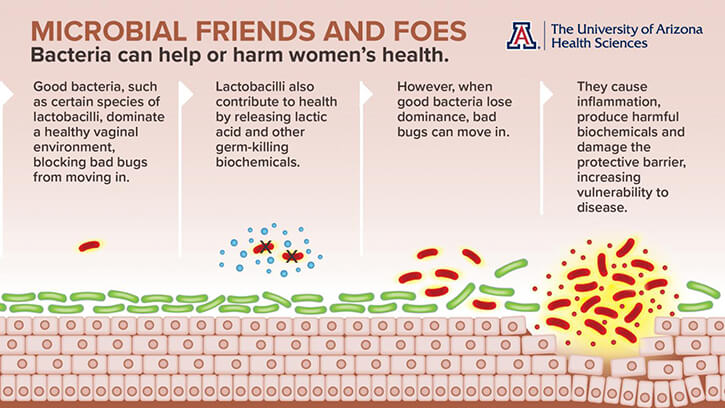
Research coming out of the Herbst-Kralovetz Lab and across the world is pointing to similar conclusions: that there are “good” vaginal bacteria that are associated with health, and “bad” bacteria that are associated with diseases like cancer. But are these “bad” bacteria causing cancer, or are they simply bystanders?
“Association versus causation is a major issue in the field,” Dr. Herbst-Kralovetz said. “These bacteria are in the specimens we collect, but the big question is, are they influencing carcinogenesis? Were they there the whole time or do they favor this new environment?”
Dr. Herbst-Kralovetz has conducted studies examining the vaginal microbiomes of women with and without cervical cancer — which is caused by a virus that is usually cleared by the immune system but can sometimes persist, leading to cancer. It turns out that “good” bacteria called lactobacilli are associated with cervical health, while “bad” bugs like Sneathia and other anaerobic bacteria are associated with the persistence of the viral infection and possibly the development of cervical cancer. Her lab has begun uncovering interesting associations between the vaginal microbiome and endometrial cancer related to pH. More optimal microbiomes are dominated by lactobacilli, which lower the vaginal pH by releasing lactic acid.
“Our studies are really preliminary right now, but we’ve seen a significant difference in the vaginal pH between women with and without endometrial cancer, which is a really low-tech way to look at the vaginal community,” Dr. Herbst-Kralovetz said. “When you have a depletion of lactobacilli, you have an overgrowth of these bad bacteria. Then you increase your pH.”
Her lab is conducting the largest study in history to investigate the connection between the vaginal microbiome and endometrial cancer. When the results are in, she hopes to shed light on whether any particular species of bacteria might be associated with the development of endometrial cancer.
“We’ve really tried to make our studies stand apart from others. Right now, we have 200 specimens. Other studies have collected 30 or 40 samples,” Dr. Herbst-Kralovetz said. “It’s taking time because I wanted to be thorough.”
Drivers and Passengers
Dr. Herbst-Kralovetz talks of cancer progression as a journey with a beginning and an end. We don’t know if the “bad” cancer-associated bacteria are along for the ride — or if they’re in the driver’s seat on the road to cancer. If Sneathia or another bug is shown to be behind the wheel, potential therapeutic interventions could be developed to target the cancer early — and force a U-turn. Scientists also would be able to devise powerful new strategies for cancer prevention by figuring out how to kill the bad bugs and replace them with beneficial bugs.

But if the so-called bad bugs are in the passenger’s seat, they might just be sitting there quietly, hoping to get to their destination: a cancerous environment where they can thrive. Once they get there, they might proliferate wildly, obscuring the actual drivers from view. If a bug is a passenger rather than a driver, targeting it for destruction wouldn’t help — but its presence could be a sign that the body is on the road to cancer.
“Using them as a potential biomarker could give us an early prediction of cancer,” Dr. Herbst-Kralovetz said. “We could intervene before cancer occurs.”
Improving Cancer Survivorship
Once someone has cancer, however, it’s too late to prevent or predict it. But even at this point, solving the mysteries of the microbiome can still help improve survival and quality of life.

There also is compelling evidence that radiation and chemotherapy can throw the microbiome out of balance — and that an off-kilter microbiome somehow interferes with these treatments, making them less effective and more toxic.
“We think these therapies probably alter the vaginal microenvironment, especially if you’re getting pelvic radiation for gynecologic cancer,” Dr. Herbst-Kralovetz said. “But we don’t have any data yet.”
That lack of data means that, so far, there isn’t a recipe to create synthetic microbial cocktails of “good” bacteria that might boost cancer treatments’ effectiveness and blunt their negative side effects.
It can take a lifetime to untangle even one of the connections between myriad species of vaginal bacteria, several types of gynecologic cancer and countless other variables. Dr. Herbst-Kralovetz says she is up to the task, because for her, this riddle isn’t just a mesmerizing brainteaser — the answers she finds will benefit anyone at risk for gynecologic cancer.
The story originally appeared on University of Arizona Health Sciences' website and was written by Anna Christensen, MPH.
About the College
Founded in 2007, the University of Arizona College of Medicine – Phoenix inspires and trains exemplary physicians, scientists and leaders to advance its core missions in education, research, clinical care and service to communities across Arizona. The college’s strength lies in our collaborations and partnerships with clinical affiliates, community organizations and industry sponsors. With our primary affiliate, Banner Health, we are recognized as the premier academic medical center in Phoenix. As an anchor institution of the Phoenix Bioscience Core, the college is home to signature research programs in neurosciences, cardiopulmonary diseases, immunology, informatics and metabolism. These focus areas uniquely position us to drive biomedical research and bolster economic development in the region.
As an urban institution with strong roots in rural and tribal health, the college has graduated more than 1,000 physicians and matriculates 130 students each year. Greater than 60% of matriculating students are from Arizona and many continue training at our GME sponsored residency programs, ultimately pursuing local academic and community-based opportunities. While our traditional four-year program continues to thrive, we will launch our recently approved accelerated three-year medical student curriculum with exclusive focus on primary care. This program is designed to further enhance workforce retention needs across Arizona.
The college has embarked on our strategic plan for 2025 to 2030. Learn more.