Identification of Biomarkers for Endometrial Cancer Shows Promise for Faster and Less Invasive Diagnosis
Endometrial cancer is the most common form of cancer of the female reproductive organs; and unlike most other cancers that are decreasing, its incidence rates have continued to grow by a rate of 1% per year for White women and 2–3% for women of all other racial/ethnic groups, according to the American Cancer Society.

Currently, the gold standard for diagnosis is an endometrial biopsy — a form of surgery without the use of a local anesthetic where tissue is removed from the patient for further testing. Though accurate, it is an inconvenient procedure that can be quite painful for the patient.
The barriers to this type of procedure extend beyond the pain and the anxiety it can cause. Access to it is often less available for women without health care and for those who live in rural areas of the state because it needs to be done in a specialized setting. For women who have suffered prior sexual trauma or have other health issues, it may require an operating room.
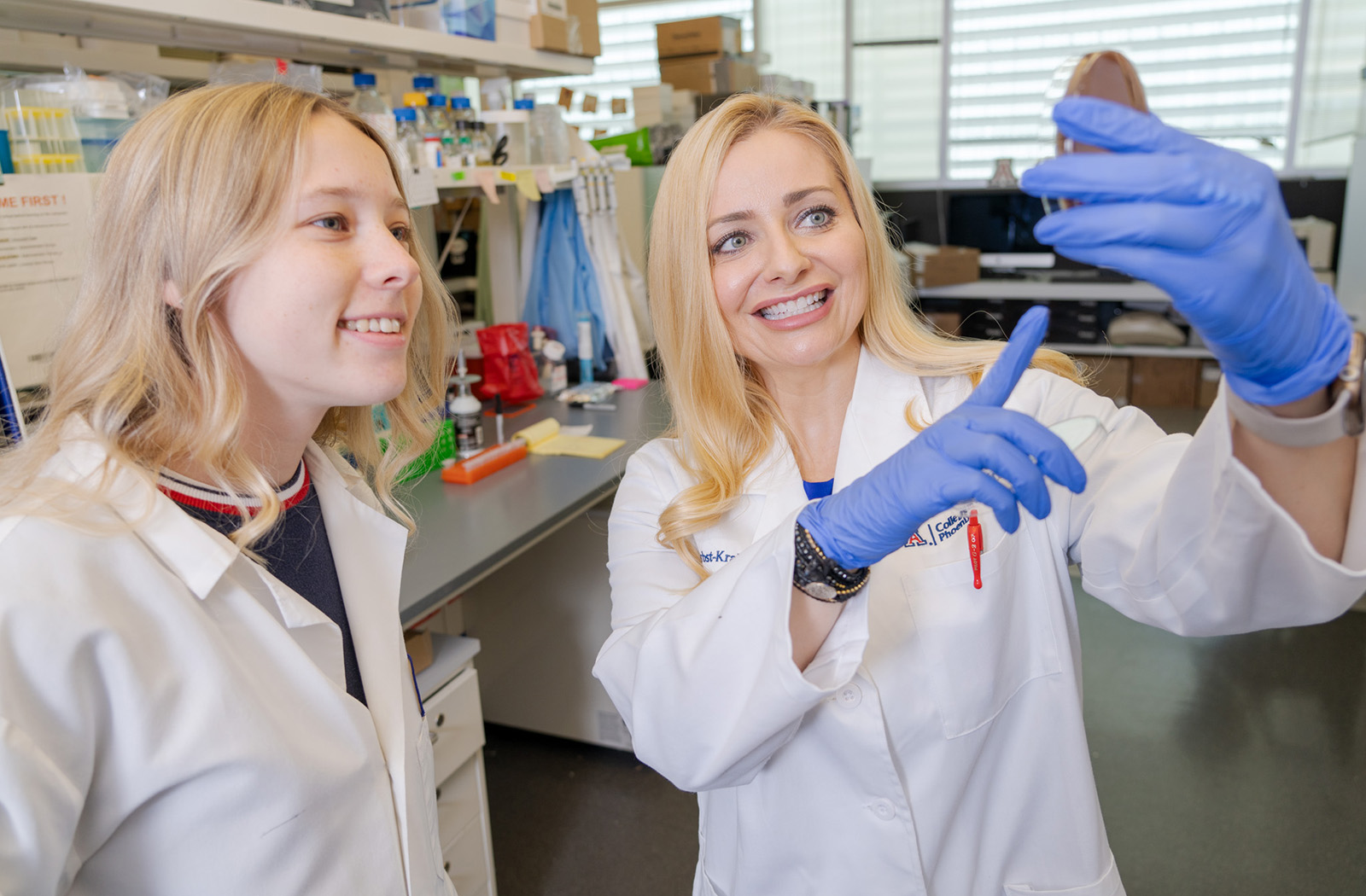
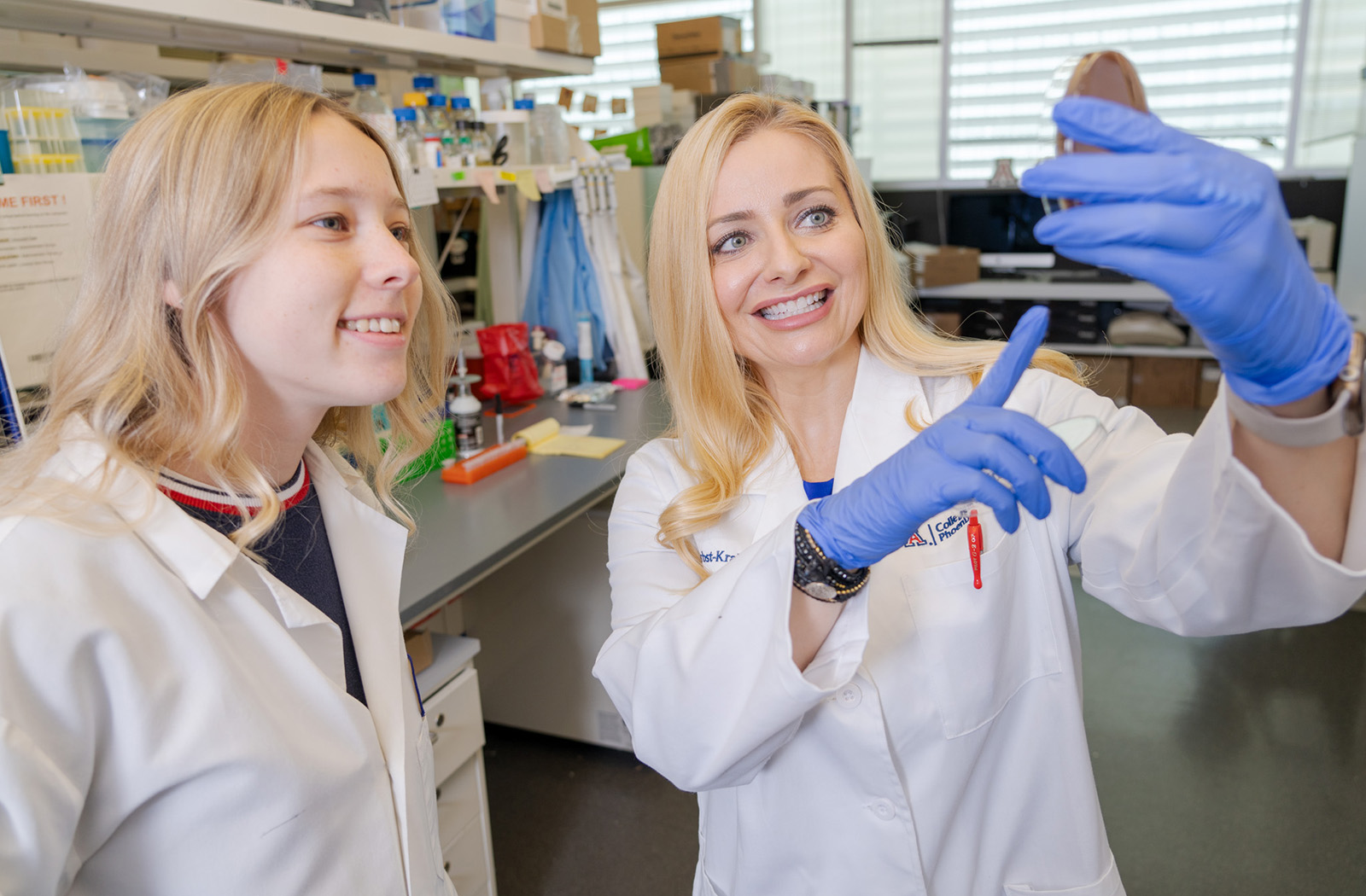
Those obstacles are “amplified within our underrepresented, understudied, minoritized populations of women — specifically here in Arizona, where Native American women and Latinas have the highest rates of endometrial cancer,” said Melissa Herbst-Kralovetz, PhD — a professor of Basic Medical Sciences and Obstetrics and Gynecology, as well as director of the Women’s Health Research Program at the University of Arizona College of Medicine – Phoenix, and a researcher with the Cancer Prevention and Control Program at the U of A Cancer Center (UACC).
Fortunately, recently published research by Dr. Herbst-Kralovetz and a highly collaborative team of UACC biostatisticians, Banner Health surgeons, gynecologic oncologists, and basic scientists demonstrated potential for a more accessible and less invasive diagnostic procedure for endometrial cancer.
Collecting samples via gentle cervicovaginal lavage from more than 190 women with endometrial cancer and non-malignant conditions, the researchers performed global untargeted metabolomics. The data they collected was then used for a multivariate biomarker discovery analysis.
The aims of the study were twofold: To identify potential biomarkers within the cervicovaginal lavages that could be used for detection of endometrial cancer and to further investigate the disruption cancer causes in the local microenvironment. “Dysregulation in metabolism is one of the hallmarks of cancer. We wanted to learn more about the pathophysiology of endometrial cancer using the sampling technique,” Dr. Herbst-Kralovetz said.

The results were more than promising. The metabolic dysregulation they discovered linked specific metabolites and pathophysiological mechanisms — including cellular proliferation, energy supply and invasion of neighboring tissues.
More promising, their research method was able to detect metabolite levels related to the overall severity the endometrial cancer presents to the patient — as in, the size and grade of the tumor. “These tumor characteristics could be used as a prognostic tool,” she said. Without surgery, “We could do this non-invasive sampling and then predict what the tumor size is, if there’s myometrial invasion, etc. That’s really important for patient risk stratification as you move forward for treatment.”
The research team’s hope is that the biomarkers will not only improve the acceptability and accessibility of diagnosis but potentially allow a patient to collect the samples themselves. These factors could lead to earlier detection of endometrial cancer.
About the College
Founded in 2007, the University of Arizona College of Medicine – Phoenix inspires and trains exemplary physicians, scientists and leaders to advance its core missions in education, research, clinical care and service to communities across Arizona. The college’s strength lies in our collaborations and partnerships with clinical affiliates, community organizations and industry sponsors. With our primary affiliate, Banner Health, we are recognized as the premier academic medical center in Phoenix. As an anchor institution of the Phoenix Bioscience Core, the college is home to signature research programs in neurosciences, cardiopulmonary diseases, immunology, informatics and metabolism. These focus areas uniquely position us to drive biomedical research and bolster economic development in the region.
As an urban institution with strong roots in rural and tribal health, the college has graduated more than 1,000 physicians and matriculates 130 students each year. Greater than 60% of matriculating students are from Arizona and many continue training at our GME sponsored residency programs, ultimately pursuing local academic and community-based opportunities. While our traditional four-year program continues to thrive, we will launch our recently approved accelerated three-year medical student curriculum with exclusive focus on primary care. This program is designed to further enhance workforce retention needs across Arizona.
The college has embarked on our strategic plan for 2025 to 2030. Learn more.