Medical Students Explore Efficacy of Potential COVID-19 Therapeutic
Three medical students at the University of Arizona College of Medicine – Phoenix are trying to improve clinical decisions for COVID-19 by consolidating the clinical and historical information available on a treatment known as Convalescent Plasma (CP) Transfusion.
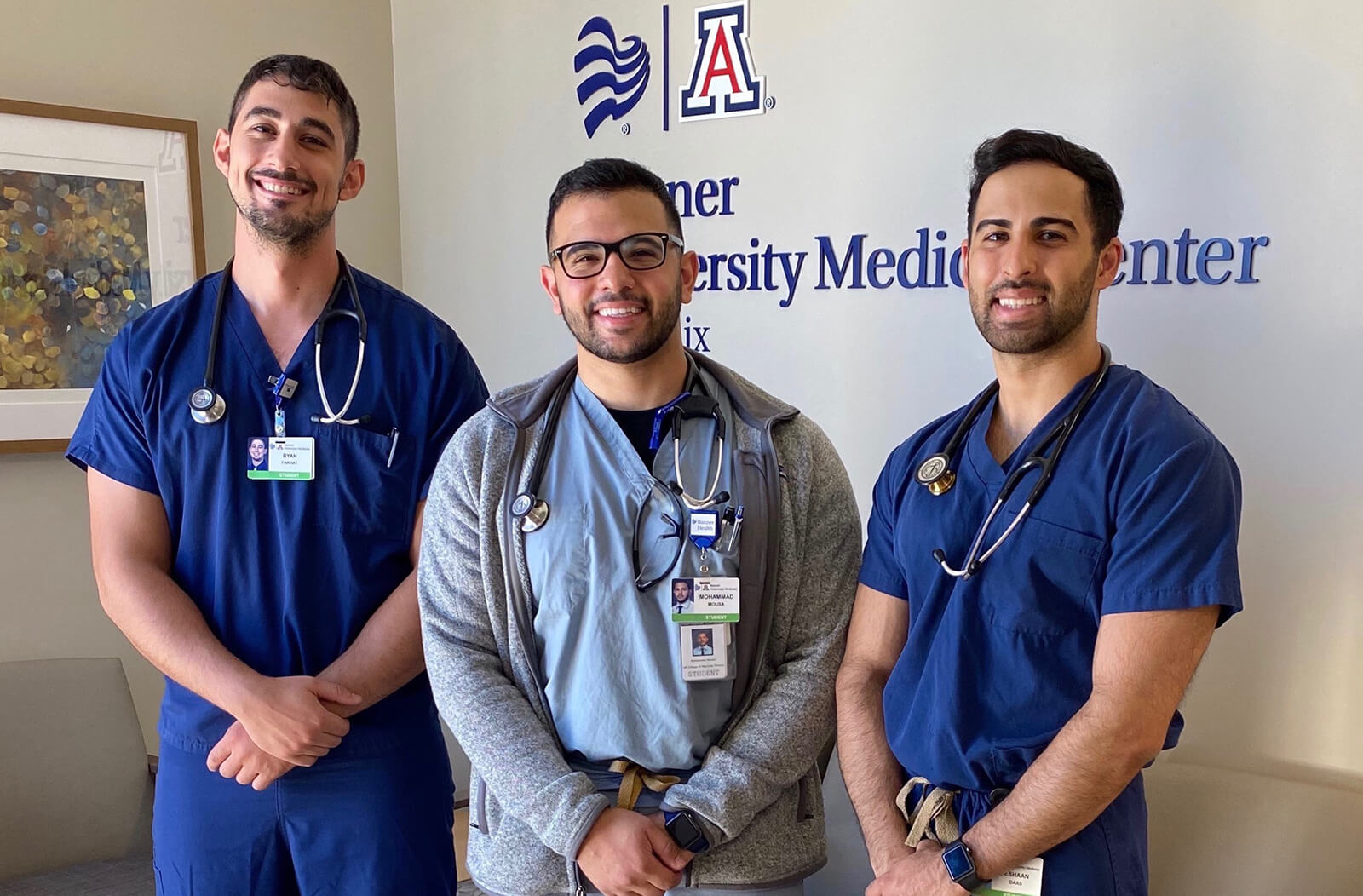
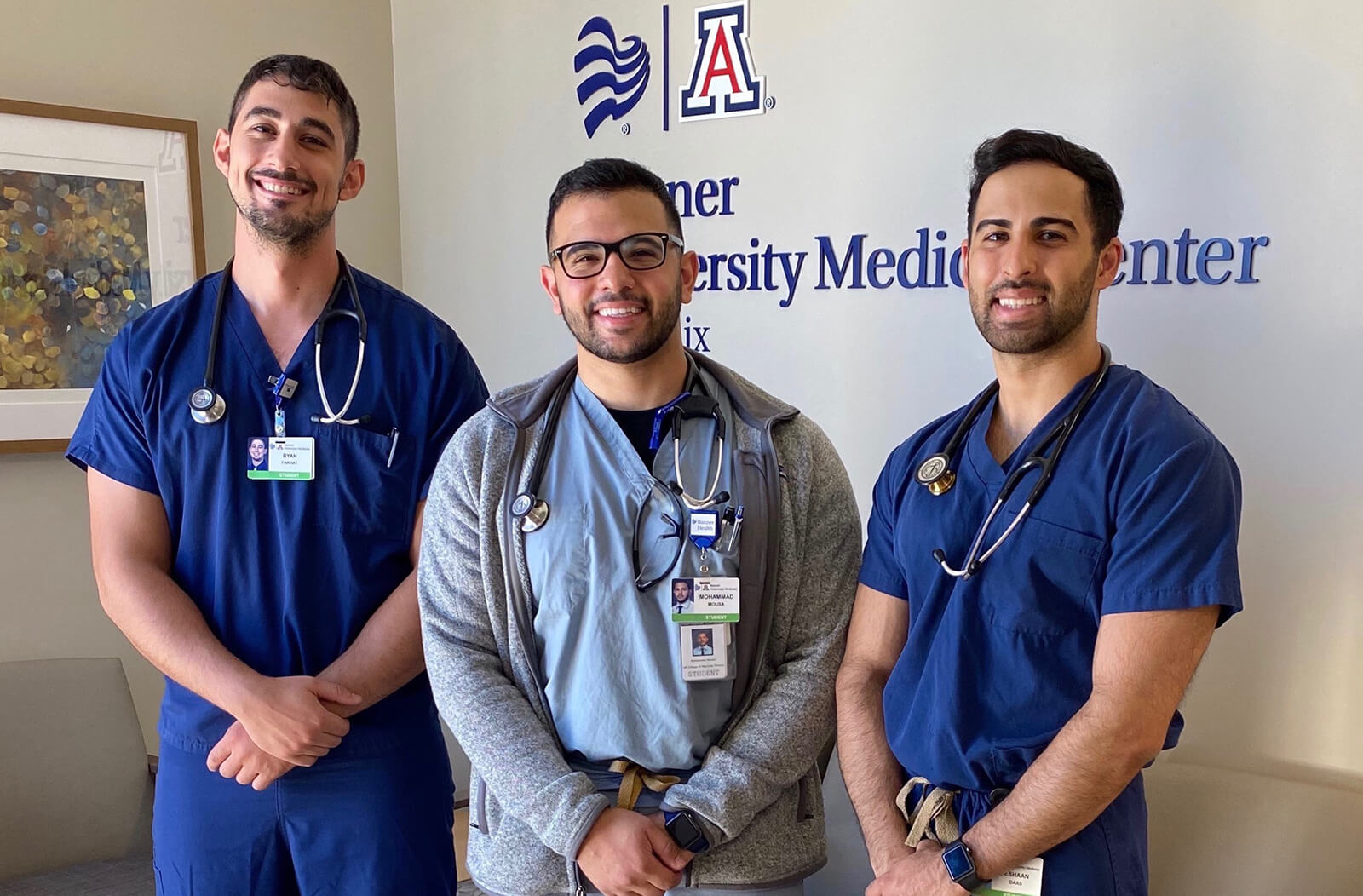
This study was led by fourth-year medical students Ryan Farhat, Mohammad Mousa and Eshaan Daas, along with their mentor Marilyn Glassberg, MD, chief of the Division of Pulmonary Critical Care and Sleep Medicine. Findings were published on July 28, 2020, in Frontiers in Medicine.

“With the rising mortality of COVID-19 and the lack of successful therapy, every possible treatment must be properly explored,” said Mousa. “CP is plasma with COVID antibodies from patients who have recovered from the virus. It has been used historically in previous virus outbreaks and a few early case reports have demonstrated that it may be beneficial for patients with active infections. CP is already being used in many hospitals around the world for those who are failing current treatment regimens. The need for a large randomized control trial is extremely necessary to determine if CP is effective.”
This project started during the initial phase of the current pandemic when the early studies in China were published. Mousa said that they were fortunate to work with Dr. Glassberg, who provided excellent mentorship and strong support during this project.
“There were a few potential therapies for COVID-19 when we started this project,” said Farhat. “We heard about hydroxychloroquine, remdesivir, azithromyocin and dexamethasone being effective in treating symptomatic patients. Convalescent plasma has been historically used to treat SARS and MERS, making us curious about its effectiveness in treating our current pandemic. We hope that the completed clinical trials can lead to an improvement in the morbidity and mortality worldwide.”
The perspective looked at the advantages of CP against COVID-19 by analyzing studies using CP during SARS, influenza pandemic and MERS, which demonstrate potential for clinical efficacy during the COVID-19 pandemic. The perspective also highlighted the limitations of CP implementation — such as transfusion of blood products, specifically plasma, being associated with a few rare adverse effects.
"Perspectives help direct future studies by identifying data that is needed to provide efficacy," Dr. Glassberg said. “Ryan, Mohammad and Eshaan had a specific question: 'Would CP be efficacious?' Our perspective suggested that more studies needed to be done, with the most recent trial suggesting that the timing and titer of neutralizing antibodies make a difference in outcome."
After evaluating the advantages and limitations of CP, the study said that there is promise in this treatment option for patients with COVID-19. They added that there are currently multiple randomized trials in progress evaluating the effectiveness of CP.
“We hope our work contributes to the advancement of our understanding of this virus and results in positive health care outcomes,” Daas said. “Lastly, while novel treatment options are explored by researchers around the world, it is still a collective duty to keep our community healthy with measures such as social distancing, wearing a mask and hand washing.”
Topics
About the College
Founded in 2007, the University of Arizona College of Medicine – Phoenix inspires and trains exemplary physicians, scientists and leaders to advance its core missions in education, research, clinical care and service to communities across Arizona. The college’s strength lies in our collaborations and partnerships with clinical affiliates, community organizations and industry sponsors. With our primary affiliate, Banner Health, we are recognized as the premier academic medical center in Phoenix. As an anchor institution of the Phoenix Bioscience Core, the college is home to signature research programs in neurosciences, cardiopulmonary diseases, immunology, informatics and metabolism. These focus areas uniquely position us to drive biomedical research and bolster economic development in the region.
As an urban institution with strong roots in rural and tribal health, the college has graduated more than 1,000 physicians and matriculates 130 students each year. Greater than 60% of matriculating students are from Arizona and many continue training at our GME sponsored residency programs, ultimately pursuing local academic and community-based opportunities. While our traditional four-year program continues to thrive, we will launch our recently approved accelerated three-year medical student curriculum with exclusive focus on primary care. This program is designed to further enhance workforce retention needs across Arizona.
The college has embarked on our strategic plan for 2025 to 2030. Learn more.