
New Training Package to Increase Awareness of Global Health Issues in Ophthalmology

A new software package will train eye specialists and students on the pathologies predominantly found in tropical and subtropical regions, in an effort to increase the awareness of global health issues in ophthalmology and eliminate preventable blindness.
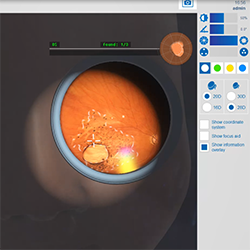
For training with the Eyesi Indirect Ophthalmoscope and Eyesi Direct Ophthalmoscope simulators, VRmagic has developed twenty new cases that feature retinal manifestations of diseases such as malaria, the Zika virus or the West Nile virus.
Robin Ross, MD, MPH, who is a clinical assistant professor in Ophthalmology and Bioethics and Medical Humanism at the University of Arizona College of Medicine – Phoenix and ophthalmologist at the Global Retina Institute, initiated the development of these global health cases for the Eyesi diagnostic simulators. This project has been five years in the making.
“Poor outcomes exacerbate gaps in care access,” Dr. Ross said. “Developing a relevant global health case series that goes beyond typical western diseases was a first step in raising awareness, inspiring interest and paving the way for a next step in building capacity in places with enormous surgical need.”
“It was said that 2020 was supposed to be the year of the eye,” Dr. Ross said. “Last year, the WHO estimated that there are 1 billion people suffering from blindness or visual impairment. In 2015, I was a part of the public health response to Ebola. As I worked on that epidemic in Liberia, I realized there wasn’t even a direct ophthalmoscope in the country, and there were no surgical ophthalmologists. The National Institutes of Health set up a clinical eye research center in Monrovia, Liberia, and we documented ocular sequelae from Ebola as well as taught ophthalmology. Throughout teaching, I realized that any simulation would have been helpful.”
When Dr. Ross arrived in Liberia, there had been 14 years of civil war that destroyed the infrastructure, so most trained ophthalmologists had been without ophthalmic equipment for years and retraining was critical to building eye care capacity. Her Liberian colleagues agreed that obtaining culturally appropriate cases and bringing simulation someday to them was an important goal.
“Almost three-fourths of U.S. academic institutions use simulation for teaching and fidelity before residents move to real patients,” Dr. Ross said. “Most low income countries lack access to simulation. It always seemed very inequitable that the least trained surgeons are left to operate on the poorest in their communities.”
Dr. Ross said that these simulations will hopefully bridge the training and knowledge gap between surgeons working in limited resource countries. She said that this was a rare opportunity to build eye care capacity and contribute to global health research.
“Only six percent of practicing ophthalmologists are underrepresented minorities,” Dr. Ross said. “Virtual ophthalmology simulation is neither privately available or available to surgeons across sub-Saharan Africa. I hope to acquire all the ophthalmology simulators in the next few years to open an ophthalmology simulation training center. Exponential growth is critical moving forward to tackle global blindness since 85 percent is preventable.”
Over the last five years, Dr. Ross has been developing this global health case series with VRmagic and many ophthalmologists and experts across the globe. She said that VRmagic saw the vision and wisdom of developing a global health case series to make teaching and training of ophthalmology cases relevant. VRmagic will provide the software to customers on request and without charge. In the future, it is also planned to implement the new cases on the Eyesi Slit Lamp simulator.
Topics
About the College
Founded in 2007, the University of Arizona College of Medicine – Phoenix inspires and trains exemplary physicians, scientists and leaders to advance its core missions in education, research, clinical care and service to communities across Arizona. The college’s strength lies in our collaborations and partnerships with clinical affiliates, community organizations and industry sponsors. With our primary affiliate, Banner Health, we are recognized as the premier academic medical center in Phoenix. As an anchor institution of the Phoenix Bioscience Core, the college is home to signature research programs in neurosciences, cardiopulmonary diseases, immunology, informatics and metabolism. These focus areas uniquely position us to drive biomedical research and bolster economic development in the region.
As an urban institution with strong roots in rural and tribal health, the college has graduated more than 1,000 physicians and matriculates 130 students each year. Greater than 60% of matriculating students are from Arizona and many continue training at our GME sponsored residency programs, ultimately pursuing local academic and community-based opportunities. While our traditional four-year program continues to thrive, we will launch our recently approved accelerated three-year medical student curriculum with exclusive focus on primary care. This program is designed to further enhance workforce retention needs across Arizona.
The college has embarked on our strategic plan for 2025 to 2030. Learn more.