Surgeon Seeks to Improve Patient’s Quality of Care with C. Difficile
Allison Tompeck, MD, hopes to change the standard of care for Clostridium difficile (C. diff) patients who undergo loop ileostomy with Vancomycin treatment by incorporating fecal transplantation into the surgical process. Her goal is to improve survival outcomes, length of stay and reoccurrence for C. diff patients.
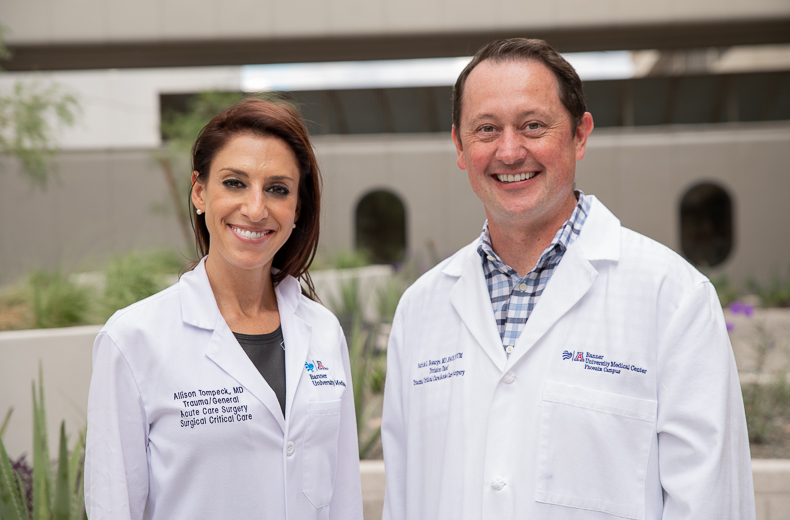
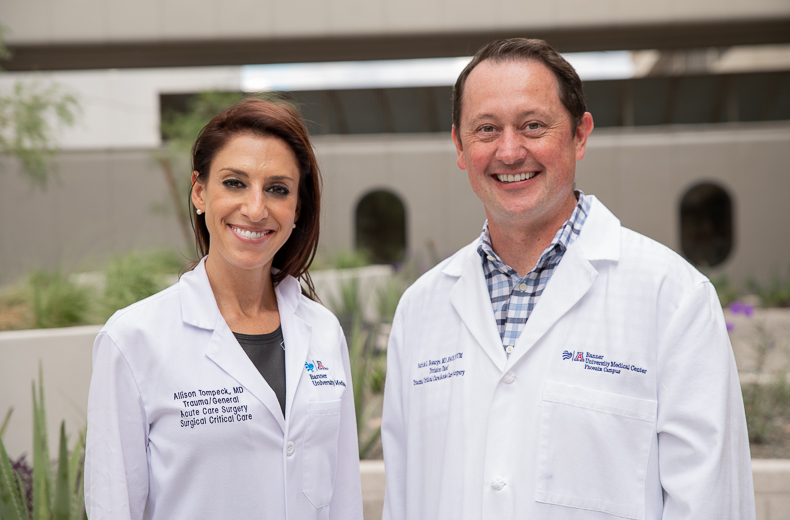
Dr. Tompeck is an assistant professor of Surgery at the University of Arizona College of Medicine – Phoenix and medical director of the Trauma Surgical Intensive Care Unit at Banner – University Medical Center Phoenix. She is working on a study with Morgan Crigger, MD, a general surgery resident at the college.
Dr. Tompeck discussed her latest research.
What is C. Diff?
C. diff is a spore-forming bacterium that causes colitis and remains the most common cause of health care-associated diarrhea. The infection causes about half a million illnesses each year in people of all ages and it can be deadly.
According to the Centers for Disease Control and Prevention, most cases of C. diff occur after a course of antibiotics. However, other risk factors include being 65 years or older, a recent hospitalization, weakened immune system and previous infection to C. diff. Symptoms develop within a few days or up to several weeks following exposure or antibiotic use, and it is contagious throughout that period.
Explain Your Research
The intestinal microbiome in a healthy adult is beneficial, providing defense against infection. Once the healthy microbiome is lost, C. diff predominates and leads to clostridium difficile-associated disease (CDAD).
For patients with C. diff acquired diarrhea and disease who do not respond to treatment despite adequate antibiotic therapy, there is an alternative treatment known as loop ileostomy with antibiotic lavage.
An ileostomy is a surgical procedure where an opening is created in the abdominal wall. Next, the lowest part of the small intestine, also known as the ileum, is looped through the opening to form a stoma. Over subsequent days, the antibiotic Vancomycin, is flushed into the colon via the ileostomy, targeting the infection.
In addition to this procedure and antibiotic treatment, there is evidence to show that fecal transplantation can restore the body’s healthy flora. In our research, we are going to see if adding the fecal transplant to the surgical procedure with Vancomycin lavage will improve outcome measures such as length of stay, time in the ICU and reoccurrence.
Why is This Important?
The incidence of C. diff is rising with the emergence of hyper-virulent strains, which infers an increased mortality risk. We need to find a better solution and improve patient outcomes.
Fecal transplantation has been quite successful in other settings for recurrent disease, as well as for patients with solid organ or bone marrow transplantation. Our study is a bit different, but it has been successful in other places, and we are very optimistic.
What’s the Goal?
The goal is simple. We want to improve the mortality rate and quality of life for these patients.
This research is supported by a seed grant awarded by the Department of Surgery at the UA College of Medicine – Phoenix. Over the last year, the department has funded five projects in the department.
About the College
Founded in 2007, the University of Arizona College of Medicine – Phoenix inspires and trains exemplary physicians, scientists and leaders to advance its core missions in education, research, clinical care and service to communities across Arizona. The college’s strength lies in our collaborations and partnerships with clinical affiliates, community organizations and industry sponsors. With our primary affiliate, Banner Health, we are recognized as the premier academic medical center in Phoenix. As an anchor institution of the Phoenix Bioscience Core, the college is home to signature research programs in neurosciences, cardiopulmonary diseases, immunology, informatics and metabolism. These focus areas uniquely position us to drive biomedical research and bolster economic development in the region.
As an urban institution with strong roots in rural and tribal health, the college has graduated more than 1,000 physicians and matriculates 130 students each year. Greater than 60% of matriculating students are from Arizona and many continue training at our GME sponsored residency programs, ultimately pursuing local academic and community-based opportunities. While our traditional four-year program continues to thrive, we will launch our recently approved accelerated three-year medical student curriculum with exclusive focus on primary care. This program is designed to further enhance workforce retention needs across Arizona.
The college has embarked on our strategic plan for 2025 to 2030. Learn more.