Second-Year Medical Student Awarded Grant to Further Scholarly Project Studying Pectus Excavatum
 Jason Raymond Jorgensen, a second-year medical student at the University of Arizona College of Medicine – Phoenix, is hoping to improve detection of physiological limitations in patients with pectus excavatum, a condition where an individual’s breastbone is sunken into his or her chest. By improving detection, Jorgensen hopes that this will lead to proper support and treatment options.
Jason Raymond Jorgensen, a second-year medical student at the University of Arizona College of Medicine – Phoenix, is hoping to improve detection of physiological limitations in patients with pectus excavatum, a condition where an individual’s breastbone is sunken into his or her chest. By improving detection, Jorgensen hopes that this will lead to proper support and treatment options.
Jorgensen is working on this research as part of his scholarly project with his mentor, Arash Sabati, MD, a clinical assistant professor in the Division of Cardiology. Jorgensen is one of three medical students who received a grant from the Valley Research Partnership (VRP) to further his research. The VRP, which is in its fifth round of funding, provided $244,230 in grants to help accelerate career development and discovery and improve health care.
Jorgensen discussed his latest research.
Describe Your Research
This project aims to determine if a 3D model of the patient's chest, generated from CT or MRI imaging, will be a better indicator of physiological limitations in patients with pectus excavatum than current techniques allow. Pectus excavatum is a deformity of the chest wall, which causes the chest bone to sink inward leading to possible compression of the heart or lungs. This deformity was thought to be cosmetic, but moderate to severe cases can also cause physiological limitations of the cardiopulmonary system. Pectus excavatum severity is currently scored using a 2D index called the Haller Index, which is a ratio between the horizontal length of the chest and the shortest distance between the vertebrae and sternum. Subsequently, there are multiple other 2D measures to quantify or describe severity. None of these ratios can accurately predict the physiological limitations a patient may experience, which is where the idea for this project came from.
Why Did You Want to Study This?
I am interested in the field of 3D modeling when it comes to patient care. Current technology allows precise 3D models to be created from CT or MRI scans that can assist physicians in a multitude of health care settings. Physicians can create 3D models that are easy for patients to understand, and surgeons can create and manipulate models to assist in preparing for surgical operations. I believe that this technology can help provide better patient care and patient outcomes if utilized properly.
Why is This Research so Important?
Pectus excavatum is the most common chest wall deformity in children, so this research is focused on a condition that is commonplace worldwide. Since this was thought of as a cosmetic lesion, we are learning more every day about pectus excavatum and its physiological impact on patients. There is a knowledge gap as multiple 2D measures have failed and this is where we hope to make impact using 3D modeling.
What Progress Have You Made with Your Research?
The progress on my research has been proceeding at a good pace. I have trained on the engineering software necessary to create the 3D computer models, and have access to the IRB approved data-set through Phoenix Children's Hospital. I have also identified the CT or MRI scans that will be used for the research project, and am currently working on generating the 3D computer models.
How Has Your Experience Been with Your Mentor, Dr. Sabati?
Dr. Sabati has been a great mentor throughout this entire project. He has taken the time, every step of the project, to ensure I understand what we are doing for the research project and why we are doing it. Even during the current pandemic when he is extremely busy with clinic work, he makes sure that I am progressing through the project and providing assistance in any way he can.
How Does the VRP Grant Help Your Research?
This grant will allow the purchase of a program called 3-matic, which helps measure displacement within the 3D computer reconstruction from CT or MRI scans. More specifically, it will take a point cloud (a set of data points in space) of the computer reconstruction of the anatomy (from the CT or MRI) to find the displacement present as a result of the chest wall abnormality from the pectus excavatum.
About the College
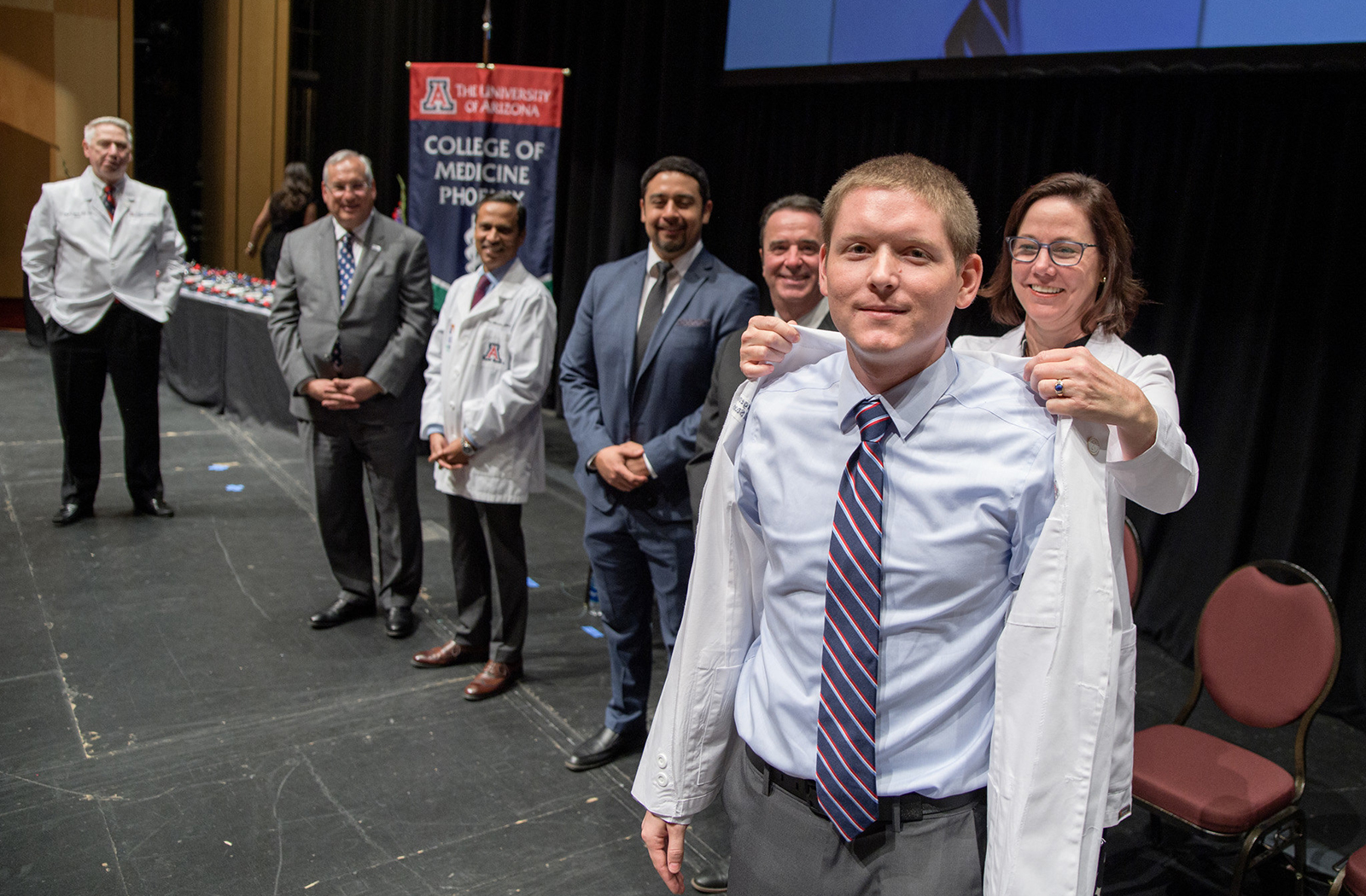
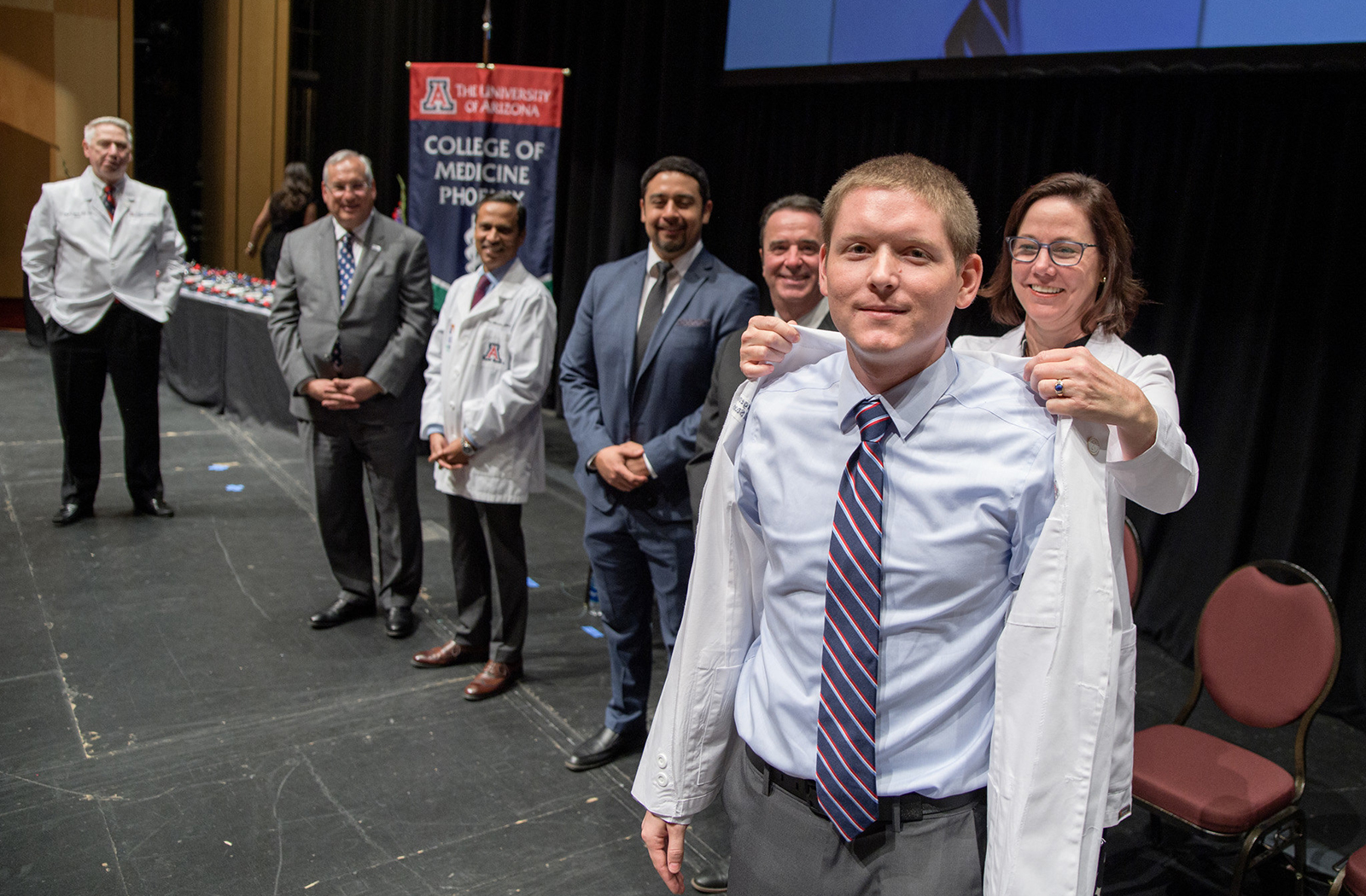
Founded in 2007, the University of Arizona College of Medicine – Phoenix inspires and trains exemplary physicians, scientists and leaders to advance its core missions in education, research, clinical care and service to communities across Arizona. The college’s strength lies in our collaborations and partnerships with clinical affiliates, community organizations and industry sponsors. With our primary affiliate, Banner Health, we are recognized as the premier academic medical center in Phoenix. As an anchor institution of the Phoenix Bioscience Core, the college is home to signature research programs in neurosciences, cardiopulmonary diseases, immunology, informatics and metabolism. These focus areas uniquely position us to drive biomedical research and bolster economic development in the region.
As an urban institution with strong roots in rural and tribal health, the college has graduated more than 1,000 physicians and matriculates 130 students each year. Greater than 60% of matriculating students are from Arizona and many continue training at our GME sponsored residency programs, ultimately pursuing local academic and community-based opportunities. While our traditional four-year program continues to thrive, we will launch our recently approved accelerated three-year medical student curriculum with exclusive focus on primary care. This program is designed to further enhance workforce retention needs across Arizona.
The college has embarked on our strategic plan for 2025 to 2030. Learn more.