
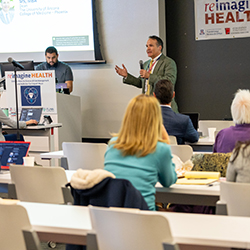
reimagine Health Research Symposium Tackled One of the United States’ Most Pressing Health Issues: Opioid Addiction

For too long, pain has been an enigma for both patients and physicians. Opioids have been used as medicines to treat pain for centuries, but new formulations and greater availability spiraled into something far worse — the opioid epidemic.
“The main objective of the symposium was to learn the most recent scientific and medical advances that have been made in our understanding of managing chronic pain, as well as how discoveries of the molecular mechanisms of addiction can inform us on how to treat opioid abuse and hopefully how to reduce deaths from opioid overdose,” said Chris Glembotski, PhD, vice dean of Research and director of the Center for Translational Cardiovascular Research.
According to the Centers for Disease Control and Prevention (CDC), more than one million people have died from a drug overdose since 1999. Most of those deaths can be attributed to opioids (75% in 2020 and 2021). It is an issue that has only compounded with time. In 2021, overdose deaths involving opioids was 10 times higher than 1999.
More alarming, as reported by the CDC and the National Center for Health Statistics, overdose deaths caused by synthetic opioids — primarily illicitly manufactured fentanyl — increased 55% from 2019 to 2020 and another 26% from 2020 to 2021. When an estimated 100 million Americans (20% of the population, as reported by the National Institute of Health’s Center for Complementary and Integrative Health) suffer from chronic pain, it is clear more needs to be done.
The symposium offered a glimpse of how it all spiraled out of control with a keynote address from Andrew Kolodny, MD — senior research scientist and medical director of the Opioid Policy Research Collaborative, Institute for Behavioral Health at Brandeis University — Responding to the Opioid Crisis: An Epidemic of Addiction.

The CDC collected data that should have been enough to stem further over-prescribing, but pharmaceutical companies took note and responded. Industry-funded “educational” messages flooded the zone, offering nonsensical counterarguments to the addictive nature of their product.
This — coupled with targeted research articles peddling industry-fed talking points and industry-backed organizations campaigning for greater use of opioids — caused confusion for physicians about the danger they were inadvertently creating for their patients.
“Regardless of how you become addicted, once you're hooked, you're not doing this because it's fun. Once you're hooked, what maintains us more than anything else, is that without the drug, you feel awful,” Dr. Kolodny said. “Patients not only feel physically ill, they truly feel like they're going to die, which is why good people will do very desperate things to maintain their opioid supply once they're addicted.”
As Dr. Kolodny finished his remarks, he did note the decline in opioid prescriptions in the U.S. over the last few years. But mortality rates have not come down. Progress and reliable treatments will take time.
Todd Vanderah, PhD — director of the Comprehensive Pain and Addiction Center, regent’s professor and chair of Pharmacology, as well as a joint professor in the Departments of Neurology and Anesthesiology at the College of Medicine – Tucson — provided a window into the future of care. In his presentation, New Avenues in the Treatment of Chronic Pain, he outlined multiple safer alternatives that are currently on the market or being assessed — such Buprenorphine (a drug that reduces the negative effects of opioids), using ultrasounds to treat chronic pain, green light therapy and cannabis.

Cannabis — and how the human body processes its chemicals through cannabinoid and endocannabinoid receptors — was the central focus of Dr. Vanderah’s presentation. Currently 48.2 million people in the U.S. (18% of the population) use cannabis, a number that has increased 43% in the past year. With use rising, it is crucial to understand how effective cannabis is as a treatment, as well as any potential side effects it may have.
His own research on the subject centers on metastatic bone cancer. An estimated 75% to 90% of patients with metastatic cancer report experiencing pain, an issue that is currently only treated with opiates. “So, I asked the question: ‘Could a cannabis product be effective in metastatic cancer pain?’” For Dr. Vanderah, the answer, pending further research, appears to be a resounding yes. Treating pain with cannabis not only inhibited pain, but reduced bone degradation.
How does this compare to when opioids were introduced to inhibit pain? Dr. Vanderah’s research showed that models with metastatic bone cancer treated with morphine experienced exacerbated progressive bone loss. The reverse effect of the model treated with cannabis. “We showed that morphine is actually causing more osteoclast, the cells that eat away the bone,” he said.
Arizona, like many other states, has suffered from the drugs devastating effects — more than 1,900 deaths from opioid overdoses occur here each year, and the numbers are increasing by nearly 10% per year.
Maria Manriquez, MD, FACOG, FASAM, PMH-C — director of the Undergraduate Medical Education Pain and Addiction Curriculum, co-medical director of the HEAL Intensive Outpatient Program at the Banner Women’s Institute and director of the Pathway Scholars Program at the college — has worked for many years to aid pregnant and parenting women suffering from substance use disorder (SUD).
Most patients she sees that are battling with SUD require not only obstetric care, but addiction medicine care and behavioral health care, as well. Dr. Manriquez has taken proactive steps to eliminate their obstacles — for example, waitlists, inadequate insurance coverage or transportation and childcare issues.

In her presentation, Success in Pain and Addiction Treatment: Overcoming Barriers to Care, she described how spreading awareness has made public perception of SUD change over time, as well as other ways to make care accessible — patient navigation and support services, financial assistance programs and insurance expansion and technology-based interventions.
“It's going to take a lot of education to help people understand that this isn't a choice; it wasn't a choice to be traumatized at some point in your life; it wasn't a choice to need to feel like you have to escape or numb yourself. Those are the realities,” she said. “It’s important to appreciate that, and then maybe we can approach this in a more humanistic manner.”
Dr. Manriquez further touched on how advocating for policy and regulatory changes at the state and national levels could further the positive progress. “Our patients are stigmatized, full of shame, often don't have the educational background to be able to be the voice they need to be. We have to be that voice for those patients,” she said. “We need to work with our legislators to amend laws and regulations and expand access to treatment options, increase funding for pain and addiction research, and then support innovative harm reduction strategies.”
The symposium also featured presentations by Wilson M. Compton, MD, MPE, deputy director of the National Institute on Drug Abuse (NIDA) of the National Institutes of Health; and John Streicher, PhD, a professor in the Department of Pharmacology at the University of Arizona; as well as a Q&A panel featuring Drs. Glembotski, Kolodny, Vanderah, Manriquez and Streicher. Sponsored by the Arizona Department of Health Services, the College of Medicine – Phoenix Translational Research Office and the Flinn Foundation — the event concluded with a networking reception in the Grand Canyon of the Biomedical Sciences Partnership Building.
Topics
About the College
Founded in 2007, the University of Arizona College of Medicine – Phoenix inspires and trains exemplary physicians, scientists and leaders to advance its core missions in education, research, clinical care and service to communities across Arizona. The college’s strength lies in our collaborations and partnerships with clinical affiliates, community organizations and industry sponsors. With our primary affiliate, Banner Health, we are recognized as the premier academic medical center in Phoenix. As an anchor institution of the Phoenix Bioscience Core, the college is home to signature research programs in neurosciences, cardiopulmonary diseases, immunology, informatics and metabolism. These focus areas uniquely position us to drive biomedical research and bolster economic development in the region.
As an urban institution with strong roots in rural and tribal health, the college has graduated more than 1,000 physicians and matriculates 130 students each year. Greater than 60% of matriculating students are from Arizona and many continue training at our GME sponsored residency programs, ultimately pursuing local academic and community-based opportunities. While our traditional four-year program continues to thrive, we will launch our recently approved accelerated three-year medical student curriculum with exclusive focus on primary care. This program is designed to further enhance workforce retention needs across Arizona.
The college has embarked on our strategic plan for 2025 to 2030. Learn more.